Overview of Stem Cell Therapy
For the past twenty-five years, researchers have made ambitious claims regarding the transformative power of stem cells in medicine. These extraordinary cells, first extracted from human embryos in the late 1990s, have an incredible capacity: they can potentially morph into any kind of tissue found in the human body. The concept was enticing—envision having spare parts available for anything that might falter in your body. Yet, the transition from theoretical laboratory possibilities to actual clinical applications revealed to be much more complicated than expected.
The discipline faced numerous years filled with overstatement, disillusionment, and even exploitation by unethical clinics. Nevertheless, following decades of diligent investigation, stem cell therapy is at last fulfilling its groundbreaking promise. Two pioneering treatments for epilepsy and type 1 diabetes are yielding astonishing results that profoundly affect patients’ lives.
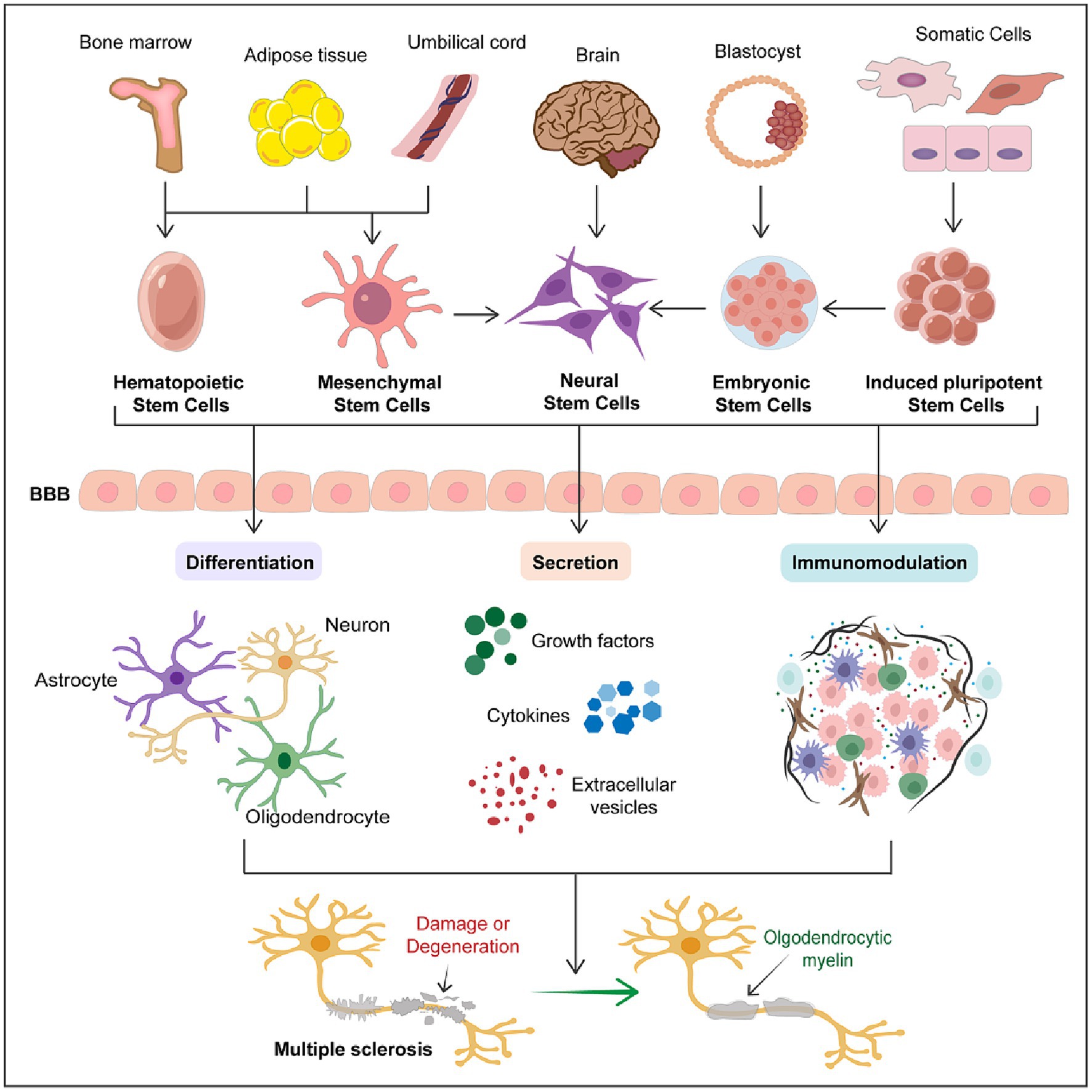
The Mechanism Behind Stem Cell Therapy
Stem cell therapy taps into the inherent capabilities of these adaptable cells to evolve into specialized tissues. Researchers utilize either embryonic stem cells or iPSCs (adult cells reengineered to function like embryonic cells). In meticulously regulated laboratory environments, they direct these stem cells to differentiate into specific cell types required for therapeutic purposes.
In the case of epilepsy therapy, stem cells transform into specialized neurons that produce GABA, a neurotransmitter that helps alleviate excessive brain activity. For diabetes treatment, stem cells evolve into beta islet cells—the insulin-secreting cells that are typically present in the pancreas but are destroyed in patients with type 1 diabetes.
After they are created, these lab-cultivated cells are implanted into patients. The cells then assimilate into the surrounding tissue and start performing their designated functions. The objective is to achieve a “functional cure” where the individual’s body can self-regulate without the need for constant medical care.
Transformational Epilepsy Treatment: The Journey of Justin Graves
Justin Graves was running a scuba diving shop in Louisville, Kentucky, when epilepsy abruptly changed the course of his life. Diagnosed at age 22 with temporal lobe epilepsy, the condition took everything—federal laws bar anyone with a history of seizures from scuba diving, ending his career. Unable to drive, he had to move and accept various jobs he could find along public transportation routes.
By 2023, at the age of 39 and two-and-a-half years sober, Graves was plagued by one to two seizures each day. When his doctors at UC San Diego proposed an experimental stem cell treatment, he readily consented. The procedure, known as NRTX-1001 and developed by Neurona Therapeutics, consisted of injecting thousands of lab-created neurons directly into his brain.
In July 2023, neurosurgeon Dr. Sharona Ben-Haim inserted a ceramic needle into his hippocampus and introduced thousands of inhibitory interneurons derived from stem cells. These specialized neurons release GABA, which may help mitigate the electrical surges that cause epileptic seizures.
The outcome surpassed expectations. Within weeks, Graves observed a significant drop in the frequency of his seizures. By early 2025, he was experiencing seizures roughly once a week, compared to daily episodes prior to the treatment. Other patients shared similar successes—one woman in Oregon had eight consecutive months seizure-free. Among the first five volunteers treated, four reported an eighty percent or greater reduction in seizure frequency. Additionally, patients exhibited cognitive enhancements, especially in memory.
For Dr. Ben-Haim, this marks a possible paradigm shift. Conventional surgical methods involve removing or damaging troublesome tissue in the brain, carrying substantial risks like memory loss and vision impairment. Providing a conclusive treatment without harming brain tissue could transform the management of epilepsy.
Innovative Diabetes Treatment: Achieving a Functional Cure
Type 1 diabetes is an autoimmune disorder in which the body attacks insulin-producing beta cells in the pancreas. Absent these cells, patients cannot manage blood glucose levels and must depend on continual monitoring and multiple daily insulin injections to survive.
In June 2024, Vertex Pharmaceuticals shared remarkable findings. Twelve individuals with type 1 diabetes who underwent an experimental stem cell therapy called VX-880 (later named zimislecel) were able to produce sufficient insulin to maintain healthy blood glucose levels ninety days following a single treatment. Impressively, three patients monitored for a full year no longer required insulin injections at all.
The treatment revolves around differentiating stem cells into functional beta islet cells, followed by administering them through a single infusion. All twelve patients who received the complete dose reached recommended blood sugar targets and sustained healthy glucose levels. Their bodies could now self-regulate in a manner they had not been capable of since their diagnosis.
This signifies a “functional cure.” Patients must take immunosuppressive medications to prevent their bodies from rejecting the new cells.