### Nanoplastics and Their Growing Influence on Drug Interactions: Consequences for Human Health and Antibiotic Resistance
In recent years, increasing recognition of environmental pollution from microplastics and nanoplastics has led to extensive studies on their impact on human health and the ecosystem. These minuscule plastic particles, arising from the degradation of larger plastic materials or from industrial processes, are now prevalent across ecosystems, food sources, water supplies, and even the air we inhale. More concerning, investigators have started to examine how these particles engage with drugs and biologically active substances, posing potential threats to medical therapies, especially antibiotics.
#### The Effect of Nanoplastics on Drug Bioavailability
Recent studies indicate that nanoplastics might affect the bioavailability, adsorption, and movement of drugs within the human body. The process of adsorption is essential, where a substance, in this instance, a drug such as an antibiotic, adheres to the surface of another material—like plastic nanoparticles. Such interactions can modify the pharmacokinetic characteristics of drugs by altering their absorption, distribution, metabolism, and eventual excretion from the human body.
In a recent investigation, a research team studied the adsorption dynamics between the broad-spectrum antibiotic tetracycline and four widely used nanoplastics: **polyethylene (PE), polypropylene (PP), polystyrene (PS), and nylon 6,6**. Tetracycline, commonly employed to treat various bacterial infections, often undergoes binding events that can lessen its availability or modify its pharmacological behavior.
##### Major Discoveries
1. **Adsorption Energies and Affinity Patterns**:
Utilizing quantum chemical computations, the research group generated over 100 potential binding configurations of tetracycline to each plastic variant. They assessed the adsorption energies of these configurations and noted that the **binding affinity differed across the nanoplastics**. Nylon 6,6 showed the highest binding affinity for tetracycline, indicating its potential significant impact on the antibiotic’s behavior. Conversely, polyethylene displayed the lowest affinity, suggesting reduced interaction.
This disparity in affinity indicates that specific nanoplastics might bind tetracycline, potentially decreasing the effective drug concentration accessible to the human body during infection treatment. Reduced drug availability could threaten therapeutic efficacy, complicating the treatment of certain conditions.
2. **Reversibility of Binding**:
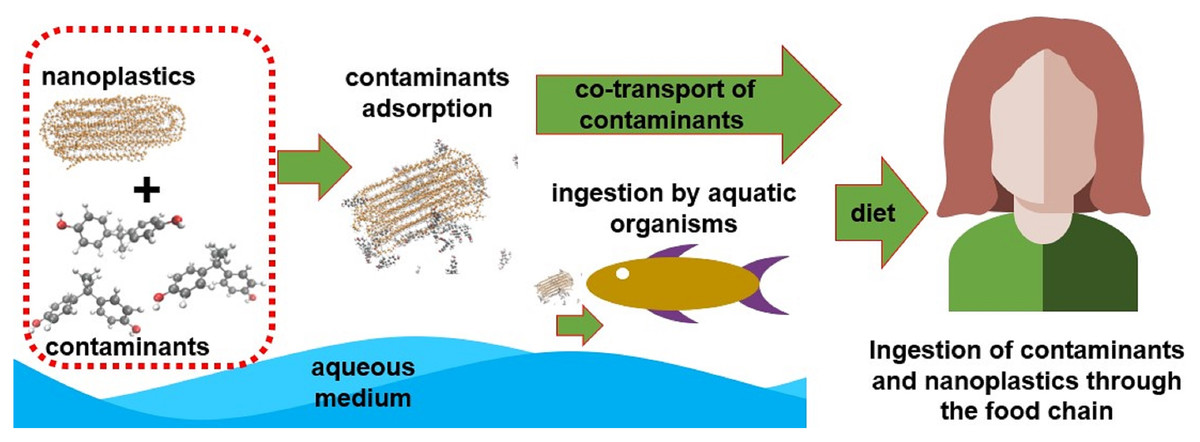
Notably, the researchers discovered that the drug’s attachment to nanoplastics could be reversed. This reversibility suggests that **tetracycline may be carried along with nanoplastics from external sources into the body**, where it could be released under certain physiological circumstances. Thus, even after an individual consumes or inhales tetracycline-contaminated nanoplastics from the environment, there is a possibility that these encapsulated drugs could subsequently be released into the bloodstream or digestive system.
3. **Possible Implication for Antibiotic Resistance**:
One of the most alarming observations from the study pertained to the localized concentration of antibiotics at the nanoplastic surface. Due to the thermodynamically favorable adsorption of tetracycline onto plastic particles, the researchers hypothesized that **local concentrations of antibiotics could be heightened at the nanoplastic interface**.
A troubling outcome of this localized drug concentration is the **increased likelihood of fostering antibiotic-resistant bacterial strains**. When bacteria encounter antibiotics at sub-lethal levels—such as in the presence of adsorbed antibiotics—they may develop resistance mechanisms. On a broader scale, the continuity of antibiotic-resistant bacteria presents a significant public health challenge, potentially resulting in infections that are more difficult to manage or entirely resistant to existing treatments.
#### Supporting Laboratory Evidence
The team performed **in vitro experiments** to investigate how this nanoplastic-drug interaction might affect biological systems. When tetracycline-sensitive cell lines were exposed to tetracycline alongside polystyrene (PS) particles, the **drug’s effectiveness was notably diminished**, indicating that these nanoparticles hindered tetracycline’s ability to kill bacteria or impede cell growth.
This observation implies that the interplay between nanoplastics and drugs, such as within tissues and cells in the human organism, **may undermine antibiotic efficacy**, raising serious concerns for medical treatment and public health.
#### Broader Consequences for Human Health and the Environment
The findings from this investigation offer significant insights regarding the potential dangers associated with the pervasive presence of nanoplastics, particularly when they interact with essential pharmaceuticals like antibiotics. The reality that **nanoplastics can sequester, transport, and potentially release drugs within biological settings** suggests that these particles could disrupt both therapeutic interventions and physiological functions in numerous ways.
Furthermore, the risk of **encouraging antibiotic resistance** is particularly alarming. As we continue to confront the global challenge of antibiotic-resistant infections, there is an urgent need to deepen our understanding of how environmental pollutants such as nanoplastics contribute to this issue.