### EMA Changes Stance: Authorizes Alzheimer’s Antibody Leqembi (Lecanemab) for Certain Patients
In a pivotal move, the European Medicines Agency (EMA) has endorsed market approval for the Alzheimer’s therapy Leqembi (lecanemab), just months after it initially turned it down. This change comes after a reevaluation of clinical evidence and is recognized as a vital advance in meeting the unmet needs of early Alzheimer’s patients across Europe. Leqembi, developed by Biogen and Eisai, had already received approval in the U.S. and Japan earlier in 2023, where it showed promise in slowing cognitive decline in early-stage Alzheimer’s by targeting amyloid plaques within the brain.
Nonetheless, while the EMA aligns with other global authorities in favoring Leqembi, this choice has sparked controversy regarding the drug’s effectiveness, safety, and economic viability, highlighting the intricacies associated with Alzheimer’s treatments.
—
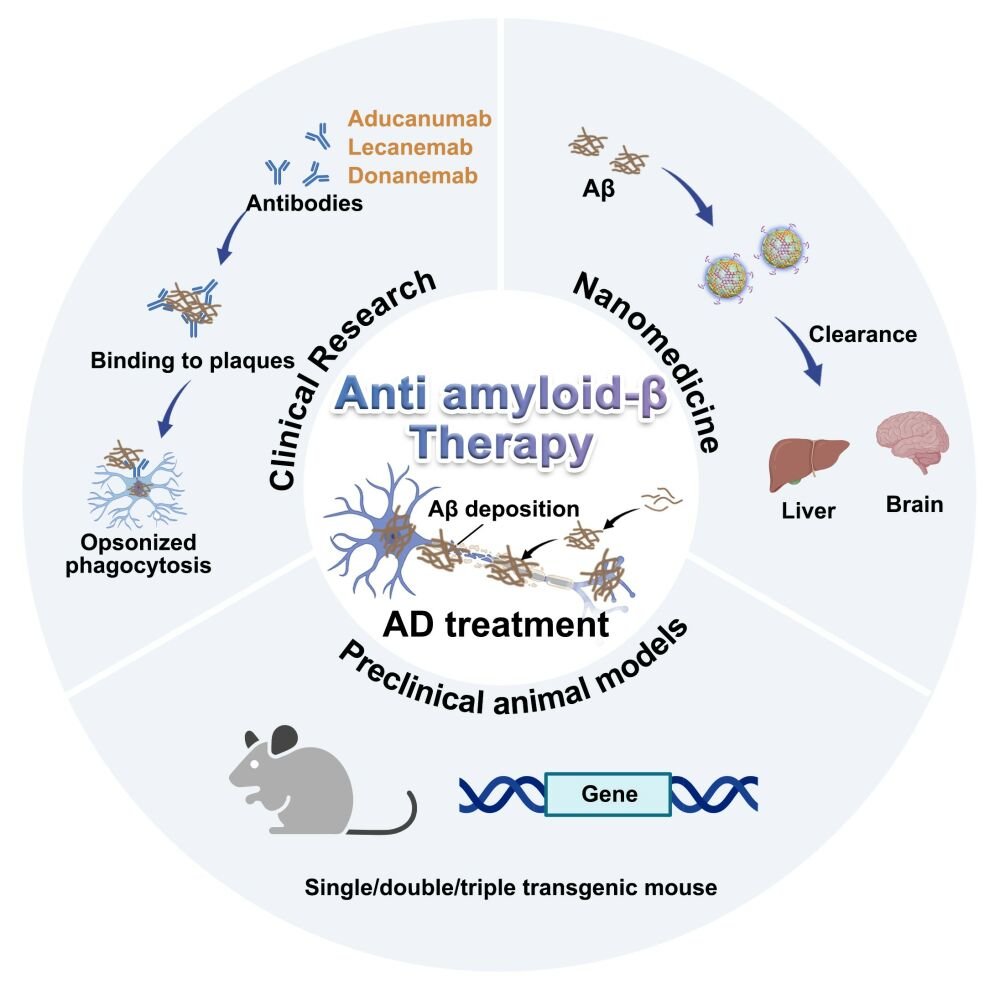
### Mechanism of Leqembi: Eliminating Amyloid Plaques
Leqembi is part of a novel category of anti-amyloid antibodies aimed at fighting Alzheimer’s by eliminating amyloid plaques—protein aggregations in the brain that are thought to aggravate the disease’s advancement. Clinical research has indicated that this medication can decelerate cognitive deterioration in patients with mild cognitive impairment or early-stage Alzheimer’s. However, its influence on overall quality of life appears limited, with critics arguing that its advantages are challenging to observe in practical, everyday situations.
Seb Walsh, a public health analyst at the University of Cambridge, remarks, “The medications effectively remove amyloid from the brain, but the implications for individuals’ cognition and life quality are minimal. After 18 months of treatment, a physician would be indistinguishable between the average patient on the medication and the average patient on placebo.”
—
### Initial Denial and Safety Issues
The EMA was initially reluctant to approve Leqembi because of concerns regarding its considerable risks, particularly amyloid-related imaging abnormalities (ARIA). These adverse effects encompass brain swelling and bleeding, evident on MRI scans in specific patients undergoing treatment. Although no fatalities due to ARIA were recorded during the 18-month clinical trials, some deaths attributed to this side effect have been reported in the United States, leading to stringent safety supervision protocols.
The EMA’s change in perspective occurred after Eisai sought a reevaluation of the data that excluded individuals with two copies of the Apoe4 gene—a genetic trait connected to a higher risk of Alzheimer’s and increased vulnerability to ARIA. This adjustment revealed that individuals with one or no copies of Apoe4 were significantly less likely to experience ARIA-related issues. In light of these discoveries, the EMA has now endorsed Leqembi for this specific group of early-stage Alzheimer’s patients, requiring MRIs before and during treatment for safety oversight.
—
### Response in Europe: A Split Alzheimer’s Community
The EMA’s ruling has garnered support from patient advocacy groups, including Alzheimer Europe and the Alzheimer’s Association, for broadening treatment avenues for patients and caregivers. “I’m pleased that we in Europe are not now being relegated to a waiting room, observing what occurs in the rest of the globe,” noted Bart De Strooper, a neuroscientist at University College London and the Crick Institute.
However, some in the medical and research fields maintain a cautious stance. Walsh and his associates have voiced concerns regarding the narrow patient demographic likely to gain from Leqembi. Only around 8% of individuals with early Alzheimer’s in the wider population would qualify under the eligibility criteria applied in the clinical trials. Moreover, critics express apprehension about the long-term dangers of administering the treatment, which necessitates biweekly infusions and continuous brain monitoring, as well as the financial burden on healthcare systems.
—
### Mixed Reactions in the UK: Cost versus Benefit
Although Leqembi received approval for use in the UK by the Medicines and Healthcare products Regulatory Agency (MHRA) in August, it will not be made available through the National Health Service (NHS). The National Institute for Health and Care Excellence (NICE) concluded that the drug’s steep price, combined with its limited benefits, does not justify its funding by the NHS. NICE pointed to the costs associated with biweekly hospital infusions, the intensive monitoring needed, and the slight cognitive improvements noted in clinical studies as barriers to broader accessibility.
De Strooper expressed regret over this outcome, arguing that it demonstrates a lack of foresight: “The UK has made a very short-sighted decision focused solely on finances and has failed to broaden its vision towards enhancing diagnostics and determining which segments of their population could benefit.”
—
### The Future of Anti-Amyloid Treatments: What Lies Ahead?
Leqembi is not the sole player in the swiftly changing anti-amyloid treatment arena. Eli Lilly has entered the scene with