**Grasping the Controversy Surrounding BPA: Safety, Science, and Public Discourse**
The discussion surrounding bisphenol A (BPA), a chemical extensively utilized in plastics and epoxy resins, remains a continuous contention among environmental advocates, consumer defenders, scientists, and regulatory authorities. The presence of BPA in common products, spanning from plastic containers to food can linings, has incited worries over its ability to leach into consumables at minute quantities, fueling fears of negative health implications. In spite of comprehensive assessments from regulatory organizations like the U.S. Food and Drug Administration (FDA) and the European Union (EU), public sentiment continues to be polarized.
This article seeks to deliver a fair and scientific viewpoint on the BPA debate, exploring why regulatory bodies uphold its safety at existing exposure levels while delving into the broader environmental and societal consequences.
### What is BPA, and Where is it Located?
Bisphenol A (BPA) is a chemical substance primarily utilized in the production of polycarbonate plastics and epoxy resins. These substances play a vital role in creating durable, heat-resistant plastics used in water bottles, food storage containers, and medical apparatus. Epoxy resins containing BPA also coat metal cans to avert corrosion and contamination.
The extensive use of BPA invariably leads to trace amounts leaching into food and drinks, especially from canned foods and those that are high in fat or acidity. Although these levels are generally measured in parts per million or billion, the risk of sustained low-dose exposure has kindled apprehension, particularly concerning hormonally active substances.
### The Central Issue: BPA as a Hormonal Disruptor
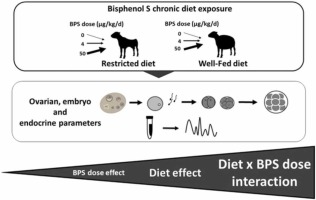
At the heart of the BPA discussion is its designation as an endocrine disruptor. BPA can simulate estrogen, an essential hormone in the human body, albeit with significantly less potency. Its structural similarity to estrogen receptors has instigated fears that it may disrupt hormonal balance, potentially leading to developmental, reproductive, neurological, and immune issues.
Particular focus has been directed toward vulnerable groups such as infants, expectant mothers, and fetuses. Opponents of BPA contend that even minimal exposures to endocrine-disrupting agents could be detrimental, especially during crucial developmental periods. The emergence of earlier studies that indicated high BPA levels in human blood and urine heightened the urgency of these concerns.
### Regulatory Evaluations: Why the FDA and EU Assess BPA as Safe
In spite of public anxiety, the FDA, EU, and various regulatory bodies globally have consistently classified BPA as safe at present exposure amounts. Their determinations are grounded in extensive scientific research and government-sponsored investigations. Here’s a summary of their reasoning:
1. **Rapid Metabolism and Elimination**: The human body rapidly metabolizes and eliminates BPA, substantially diminishing its capacity to accumulate to harmful levels. After ingestion, BPA is swiftly absorbed and processed by the liver, transforming it into inactive and water-soluble metabolites. These metabolites are expelled in urine within hours. Importantly, less than 1% of ingested BPA remains in an active form, rendering it highly improbable to produce estrogen-like effects at current exposure levels.
2. **Minimal Dietary Exposure**: Evidence from studies on food consumption indicates that the average BPA intake in adults is significantly beneath established safety limits. For example, a 70-kilogram adult is estimated to ingest less than 70 micrograms of BPA each day—this is a small fraction of amounts judged harmful, even under sensitive risk evaluations.
3. **Errors in Earlier Research**: Preliminary studies that indicated elevated BPA levels in blood samples from the general population likely suffered from contamination during sample handling or analysis. This misstep originated from the use of BPA-containing plastic laboratory equipment, which could leach small amounts of the chemical into testing samples. When contamination was mitigated, more rigorous investigations reliably found BPA at undetectable concentrations in human blood.
4. **Limited Estrogenic Activity**: The capacity of BPA to imitate estrogen is thousands of times weaker than the body’s natural estrogen, estradiol. Even if BPA were to attain measurable levels in the bloodstream, its estrogenic impact would remain trivial. Animal studies, where subjects are often exposed to dosages hundreds or thousands of times greater than those typically encountered by humans, have found no significant health repercussions.
5. **Safety in Pediatric Groups**: Although infants and young children possess underdeveloped liver and kidney functions, recent research suggests that their ability to metabolize BPA is nonetheless adequate to avert harmful accumulation. Findings from studies involving baby monkeys, often utilized as models for human infants, reinforce the conclusion that BPA exposure in infants is minimal and swiftly processed.
### The Enduring Public Distrust
Despite scientific data endorsing BPA’s safety at existing exposure levels, public distrust continues to prevail. Critics, including influential individuals like New York Times columnist Nicholas Kristof, accuse regulatory agencies such as the FDA of yielded influence from “Big Chem” and neglecting public health responsibilities.
This skepticism stems partly from a broader societal suspicion concerning industry impact on public policy. Moreover, the intricate nature of toxicology research and risk assessment can leave laypeople grappling with conflicting narratives. The precautionary principle—the belief that we