A Milestone in Cardiac Treatment: New Self-Sustaining, Bioresorbable Pacemaker Brings Fresh Optimism After Heart Surgery
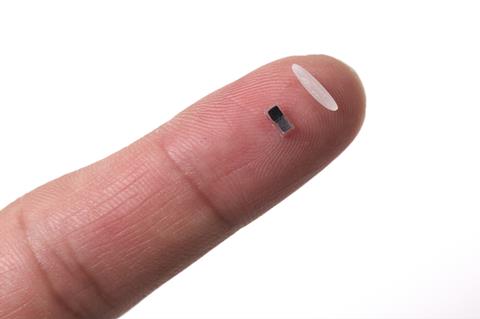
In a noteworthy advancement in cardiac healthcare, a global consortium of researchers has introduced an innovative temporary pacemaker that is self-sustaining, bioresorbable, and compact enough to be inserted through a hypodermic needle—measuring just a few millimeters in diameter, akin to the size of a grain of rice. This extraordinary device holds the potential to greatly enhance recovery outcomes for patients undergoing heart surgery, especially young children.
The Issues with Traditional Temporary Pacemakers
Patients who experience major cardiac surgery—particularly procedures necessitating a temporary cessation of the heart—often depend on a temporary pacemaker to stabilize heart rhythms during the crucial recovery phase. Current devices depend on slender wires, or leads, that connect implanted electrodes to an outside power source. Although they are effective, these leads can become integrated into scar tissue over time. Their removal later can unintentionally harm healthy heart tissue, sometimes resulting in fatal consequences.
John Rogers, a biomedical engineer at Northwestern University and the chief developer of this new device, notes that this scenario can result in severe internal bleeding. The unfortunate passing of astronaut Neil Armstrong, reportedly linked to complications from the removal of temporary pacemaker leads, highlights the dangers connected with existing methods.
Harnessing Energy from Body Biochemistry
The innovative design of the new pacemaker removes the necessity for external wires and power sources. Instead, it captures energy directly from the body. Central to this technology are minuscule, 2mm-scale electrodes crafted from metals with varying electronegativities. Once implanted into heart tissue, these electrodes produce electrical energy using the body’s own biofluids as electrolytes, functioning much like a battery.
This generated electricity powers a key component: a phototransistor acting as a switch. In its inactive state—without any external prompting—the phototransistor keeps the pacemaker off. However, when irregular rhythms are detected, the system can remotely activate the pacemaker using pulses of near-infrared light.
Light-Activated Control with an External Monitor
Attached to the patient’s skin is a rechargeable lithium-polymer battery unit that perpetually monitors heart rhythms through electrocardiograms (ECGs). Upon identifying an unusual rhythm, this external unit sends out a pulse of near-infrared light—a wavelength capable of penetrating biological tissue. This light triggers the pacemaker’s phototransistor, completing the circuit and allowing electrical current to flow across the heart’s surface, prompting it to contract.
Benefits Over Current Devices
Rogers and his team have crafted the device incorporating multiple benefits:
1. Bioresorbable: The pacemaker operates for several days or weeks—depending on the metallic components utilized—and safely dissolves within the body over one to three years. The residual trace materials are biocompatible and non-toxic.
2. Minimally Invasive: At merely a few millimeters in width, the device can be implanted using a syringe. No surgery is required for removal since the device degrades naturally.
3. MRI Friendly: Unlike many implanted devices, the new pacemaker is devoid of ferromagnetic materials, making it safe to use with magnetic resonance imaging (MRI).
4. Multi-Site Synchronization: Light-based activation permits targeted stimulation at various cardiac locations, which is particularly advantageous for achieving synchronized pacing—usually challenging with traditional pacing systems.
Outstanding Potential in Pediatric Care
Temporary pacemakers are almost universally necessary in pediatric cardiac surgeries, but the smaller hearts of children make traditional leads more susceptible to risks. The compact size, solubility, and gentle implantation of the new device render it ideally suited for younger patients—potentially lessening mortality and complications during recovery.
Pathway to Clinical Application
Although the innovation is groundbreaking, it will undergo thorough scrutiny before widespread implementation. “It typically takes five to seven years to secure regulatory approval, even for standard devices,” remarks Rogers. Nevertheless, the team is hopeful: animal testing has yielded promising outcomes, and they have already demonstrated the device’s efficacy in hearts donated for research. They are now pursuing permission for clinical trials in living human subjects.
Expert Opinions and Future Avenues
Biomedical engineer Alex Abramson from Georgia Tech commends the research as a significant breakthrough. “The application of light renders this method more accessible than triggers based on ultrasound,” he highlighted. He was particularly impressed by the capacity for synchronized pacing across multiple heart regions. However, he cautioned that light’s limited penetration depth (up to 40mm) could limit the device’s effectiveness in certain adult patients and noted that frequent pacing demands might reduce the device’s lifespan.
Despite these challenges, this innovation heralds a promising new chapter in bio-integrated, temporary cardiac support. As the research progresses toward human trials and potential commercialization, this diminutive, self-sustaining pacemaker could considerably diminish post-operative complications and enhance outcomes—particularly for the most vulnerable patient populations.
In the dynamic realm of biomedical innovation, this development may signify the dawn of safer, smarter heart care.