Groundbreaking USC Brain Imaging Study Reveals Causes of Urinary Incontinence in Stroke Survivors
An innovative study by researchers at the University of Southern California (USC) has uncovered the neurological foundations of a commonly overlooked yet serious outcome of stroke: urinary incontinence. Featured in the journal Stroke, the research offers the most thorough perspective to date on how particular brain networks—especially the salience network—dysfunction in stroke patients, resulting in loss of bladder control.
A Widespread Yet Underestimated Post-Stroke Issue
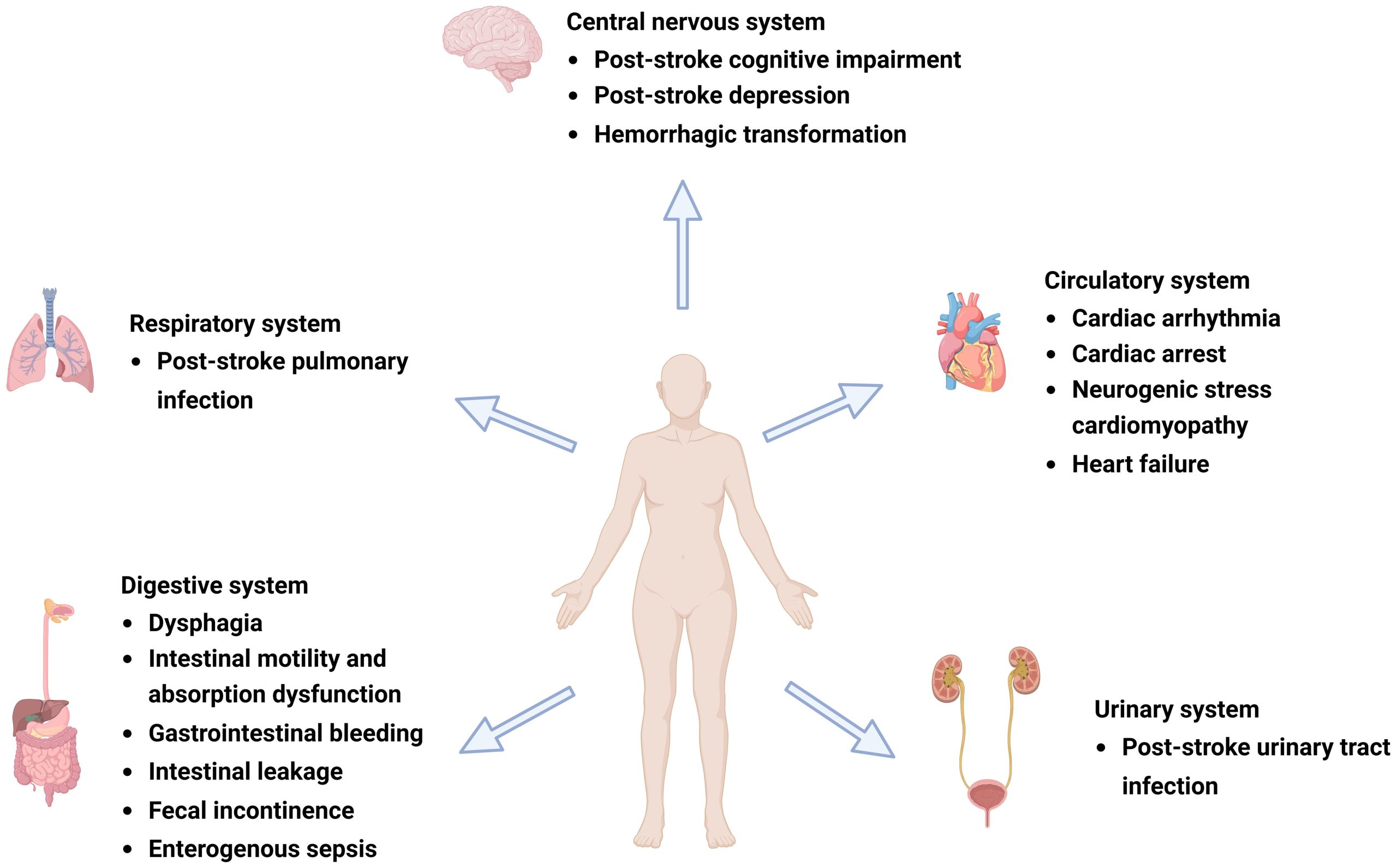
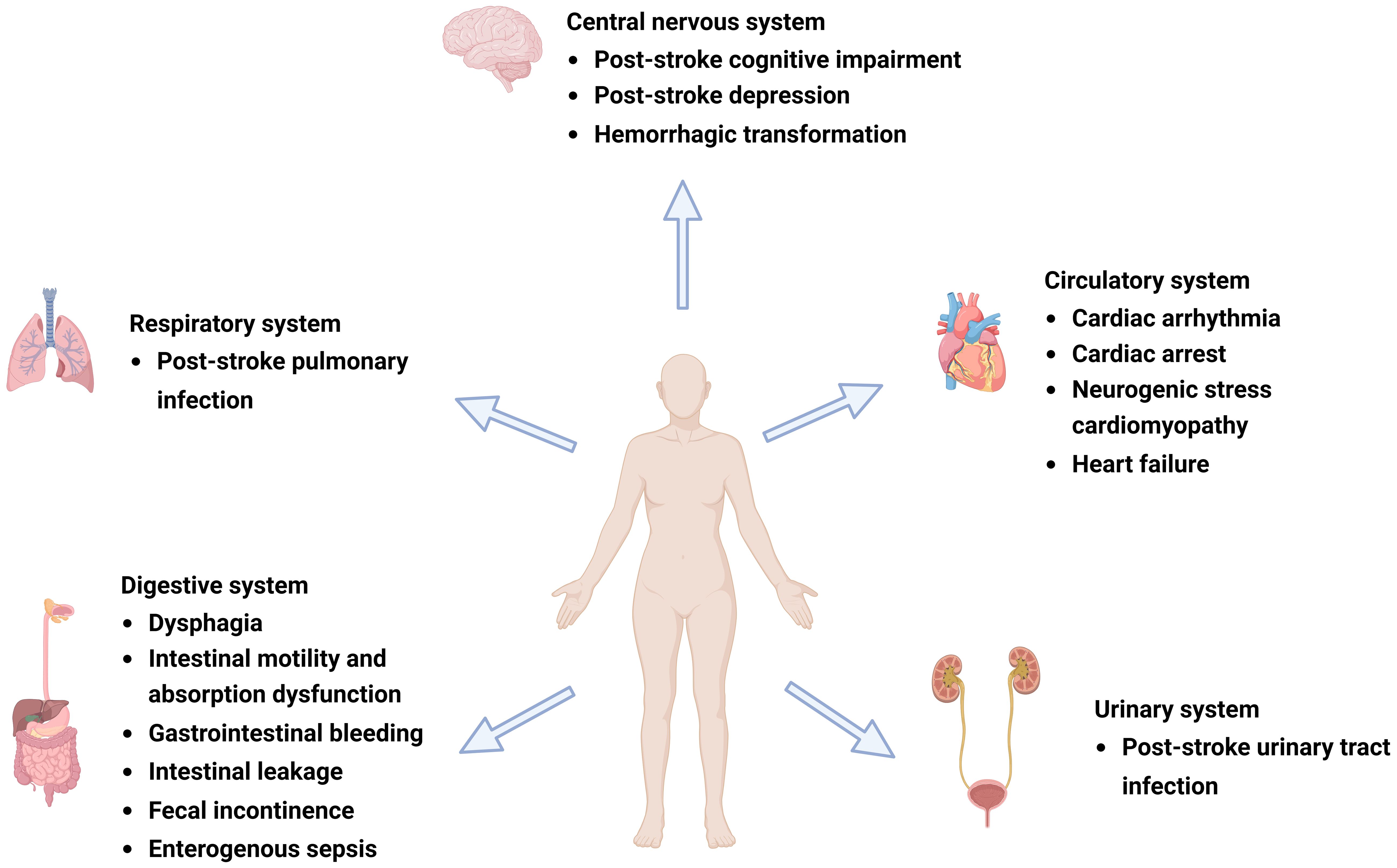
Up to 79% of stroke survivors experience urinary incontinence immediately after their event, with nearly 40% continuing to be affected a year later. More than just a nuisance, post-stroke incontinence considerably increases the risk of death and disability and correlates with poorer overall recovery outcomes. Yet, it remains one of the most neglected areas in stroke rehabilitation approaches.
Dr. Evgeniy Kreydin, the lead author and an adjunct assistant professor of clinical urology at the Keck School of Medicine of USC, emphasizes the brain’s critical role in managing bladder functionality.
“The brain is pivotal in regulating bladder activity, allowing individuals to perceive bladder fullness and to control urination until it is socially acceptable or to initiate it voluntarily,” Kreydin stated. “Conversely, stroke survivors often find it challenging to inhibit involuntary bladder contractions and may even lose the sensation of bladder fullness completely.”
Innovative Methodology: Capturing the Hidden
Conventional studies on bladder control typically require patients to come to imaging sessions with full bladders and to empty on cue—a method that does not accurately reflect involuntary bladder activity. The USC team utilized an innovative functional magnetic resonance imaging (fMRI) technique, developed in collaboration with the USC Mark and Mary Stevens Neuroimaging and Informatics Institute.
By integrating real-time imaging with concurrent bladder pressure monitoring, the researchers could observe the brain’s activity across various cycles of bladder filling and voiding. This enabled, for the first time, the recognition of distinct neural patterns related to both voluntary and involuntary bladder actions.
“In contrast to earlier studies… our research allowed for repeated observation of filling and emptying,” remarked Dr. Kay Jann, an imaging specialist who contributed to the study. “The simultaneous recording of bladder pressure permitted us to differentiate between voluntary and involuntary bladder emptying, allowing us to identify variations in brain activity during involuntary emptying for the first time.”
Highlighting the Salience Network
The study’s most striking finding centers on the salience network—a group of interconnected brain regions that evaluate the significance of internal bodily signals and aid in decision-making. In healthy individuals, this network becomes highly active during bladder filling, assisting individuals in determining when and where it is appropriate to urinate.
In stroke survivors, while the salience network was still active during intentional bladder control, it did not activate during involuntary urination instances. This lack of neural activation during involuntary voiding indicates a failure in the brain’s ability to interpret internal signals and respond behaviorally, such as delaying urination until the right moment.
This neurological misfiring not only results in incontinence but also highlights a specific area and mechanism in the brain that could be targeted for treatment.
Consequences for Treatment and Hope for Millions
“This represents a significant milestone in grasping this frequently overlooked facet of stroke recovery,” stated Dr. Charles Liu, the senior author of the study and director of the USC Neurorestoration Center.
Identifying a consistent neurological pattern associated with incontinence opens the door to new therapeutic approaches. Potential interventions might encompass:
– Non-invasive brain stimulation aimed at the salience network.
– Medications intended to enhance neural connectivity and responsiveness.
– Cognitive-behavioral therapies focused on retraining brain responses to bladder signals.
“Further research will be essential for the neurorestoration of the urinary and reproductive systems,” Liu continued. “This work not only enriches our understanding of a common post-stroke complication but also instills hope for improved quality of life for millions of stroke survivors worldwide.”
Recognized Achievement
For its significant contributions to neuro-urology, Dr. Kreydin received the esteemed McGuire-Zimskind Award from the Society of Urodynamics, Female Pelvic Medicine, and Urogenital Reconstruction.
A Collaborative Initiative
This research involved a multidisciplinary team of professionals, including experts in urology, neurosurgery, and neuroimaging, from the Keck School of Medicine of USC, Keck Medicine of USC, Rancho Los Amigos National Rehabilitation Center, and the Shirley Ryan Ability Lab.
Future Directions
While the primary focus remains on post-stroke incontinence, the researchers remain optimistic that their findings will direct subsequent studies into other neurological origins of bladder dysfunction, such as Parkinson’s disease and multiple sclerosis.
Future investigations may also examine how varying types and severities of stroke affect the salience network and whether early targeted interventions could help avert long-term complications.