A Fresh Perspective on Parkinson’s Diagnosis: Retinal Assessments May Transform Early Identification
An ordinary eye examination might soon serve a purpose beyond just evaluating your eyesight — it could also play a crucial role in identifying neurological conditions well ahead of symptom onset. Recent findings by researchers at Université Laval in Canada have revealed a significant correlation between alterations in the eye and the initial phases of Parkinson’s disease. Their discoveries indicate that routine retinal evaluations could become a revolutionary method for early diagnosis, potentially altering treatment results for millions globally.
Detecting Parkinson’s Before Symptoms Appear
Parkinson’s disease, a progressive neurodegenerative condition that impacts movement, generally manifests through signs like tremors, rigidity, or reduced mobility. Nevertheless, scientists estimate that by the moment these motor symptoms become noticeable, the illness has often been active for several years — a period during which irreversible harm has already taken place.
“The problem with Parkinson’s is that once an individual seeks medical advice due to tremors or other motor complications, the neurons that facilitate movement have typically already entered a degenerative and untreatable phase,” states Martin Lévesque, the lead author of the study and a professor at Université Laval’s Faculty of Medicine as well as a researcher at the CERVO Brain Research Centre.
But imagine if Parkinson’s could be identified prior to the emergence of any observable symptoms?
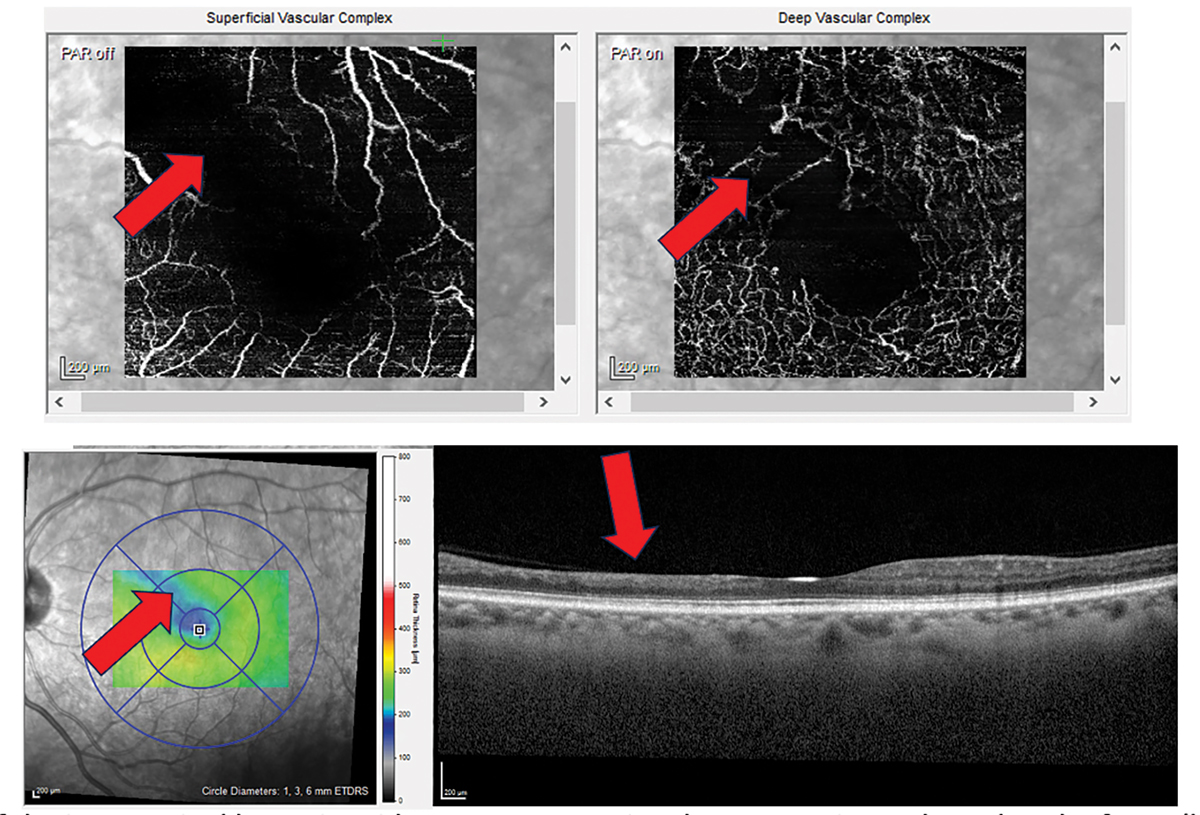
The Retinal Indicators of Parkinson’s
In a pioneering study featured in the journal Neurobiology of Disease (May 2024 issue), the Université Laval research group utilized a method known as electroretinography (ERG) to detect specific electrical patterns in the retinas of individuals at early stages of Parkinson’s disease. ERG is a non-invasive procedure that evaluates the electrical response of the retina to various visual stimuli such as light flashes.
Researchers examined 20 newly diagnosed Parkinson’s patients alongside 20 healthy age-matched controls by placing small electrodes on their lower eyelids and exposing them to a range of light flashes differentiated by color, intensity, and frequency.
“Individuals with Parkinson’s exhibited a unique retinal signature — a distinct pattern of electrical activity that differed significantly from those who were disease-free,” remarks Lévesque. These findings weren’t restricted to human subjects; analogous changes were observed in Parkinson’s mouse models, bolstering the credibility of the results.
Differences Between the Sexes Providing New Understanding
Notably, the research also revealed sex-specific differences in retinal responses. Female participants demonstrated more pronounced changes in retinal activity compared to males — a finding that could illuminate how Parkinson’s disease varies in terms of prevalence, onset, and progression across genders.
This element of the study could lead to the development of more tailored diagnostic and treatment approaches in the future.
Retina: A Gateway to Brain Wellness
The retina — the delicate layer at the back of the eye responsible for light detection and sending signals to the brain — is, in fact, a component of the central nervous system. This anatomical feature positions the eye as a “gateway to the brain,” providing a unique opportunity for non-invasive observation of neurological modifications.
Specifically, the researchers observed reduced activity in bipolar cells, a crucial type of retinal nerve cell, in both human and mouse subjects displaying early Parkinson’s symptoms. In mice, they even discovered that alpha-synuclein — a protein heavily associated with Parkinson’s — collected in the retina before it was detectable in the brain.
“This indicates that the retina could function as an early alert system,” explains lead author Victoria Soto Linan, a doctoral student at Université Laval. “Through routine retinal examinations, we might identify Parkinson’s well ahead of significant brain injury.”
An Innovative Non-Invasive Screening Technique for the Future
Given the encouraging findings, the researchers suggest integrating retinal screenings into standard healthcare practices, especially for individuals aged 50 and over.
“By identifying the disease in its early stages, we can provide interventions that may halt or slow the degeneration of neurons involved in Parkinson’s,” comments Soto Linan.
Early identification paves the way for potentially life-changing outcomes, such as the initiation of protective therapies that could enhance quality of life and postpone or lessen symptom severity.
Beyond Detection: Monitoring Progress and Informing Treatment
The function of the retina may extend beyond revealing early indicators. The research group opines that retinal testing could eventually serve as a method to track disease evolution and assess how patients respond to emerging treatments — giving healthcare providers a dynamic and accessible “gauge” of neurological health.
Implications for Other Neurological Disorders
The study contributes to the growing body of evidence suggesting that vision-based evaluations could also assist in diagnosing additional brain illnesses. Comparable retinal biomarkers are under investigation for Alzheimer’s, multiple sclerosis, and even schizophrenia.
As healthcare professionals strive for earlier detection and timely intervention for diseases, instruments like retinal screening — which are quick, cost-effective, and readily accessible — could become integral to a new framework in neurological care.
A Pivotal Advancement for the Parkinson’s Community
Currently, more than 10 million individuals globally are affected by Parkinson’s disease, with most diagnoses occurring only after substantial neurodegeneration has already occurred. If validated by larger studies and adopted into clinical practice, retinal testing could redefine how and when the disease is recognized, providing hope for