Title: Ultrasound-Activated 3D Printing of Polymers Within the Body Paves New Avenues in Healthcare
An innovative ultrasound-driven technology is reshaping the realm of in situ bioprinting, allowing for the internal creation of biocompatible polymers deep inside living tissue—eliminating the need for invasive procedures or harm to neighboring cells. This groundbreaking method, already demonstrated successfully in animal studies, suggests potential future uses in targeted drug delivery, wound repair, personalized implants, and even bioelectronics.
The Drawbacks of Conventional In Vivo Printing
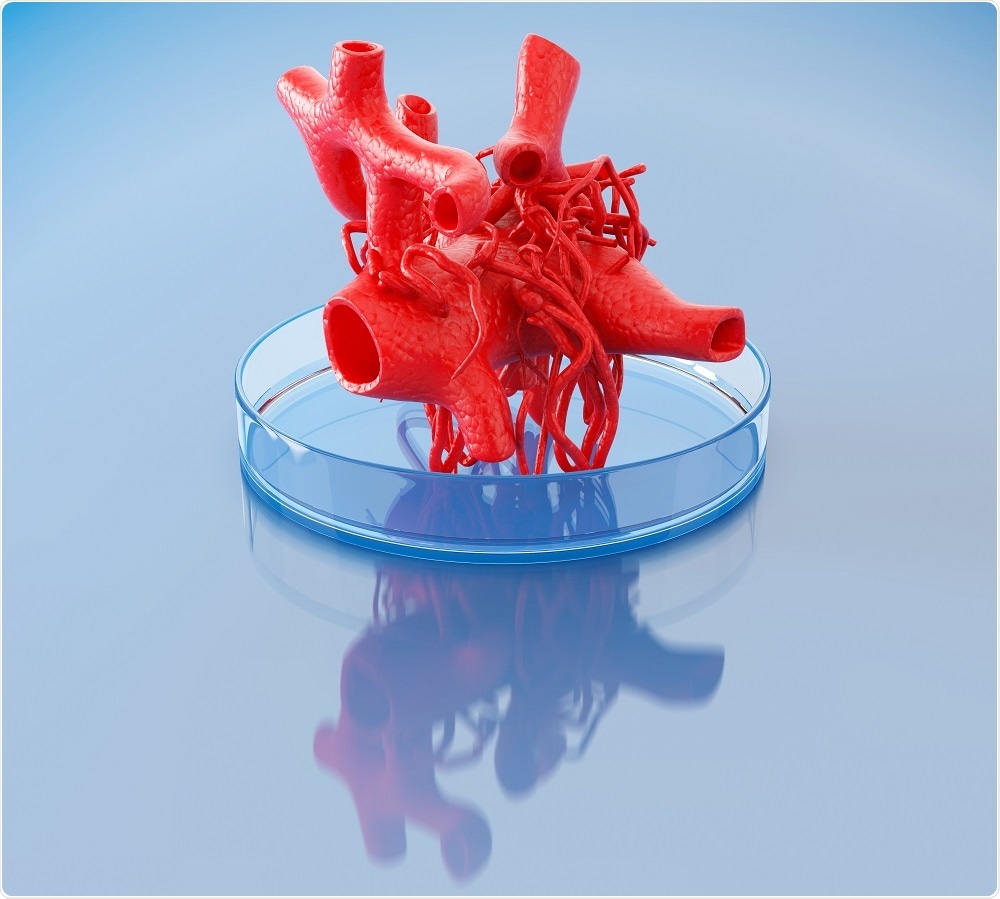
Three-dimensional (3D) printing has already transformed contemporary medicine, making it possible to create patient-specific implants, prosthetics, and biological scaffolding. However, standard additive manufacturing techniques necessitate that materials be printed externally and then surgically placed inside the body—an operation linked with risks like infections, immune rejection, and healing delays.
A recent alternative that has been investigated is light-activated polymerization, which uses near-infrared (NIR) light to cure injected bio-inks. Nonetheless, this method is limited due to the shallow penetration of NIR light through living tissue. Layers of skin, muscle, and organs rapidly attenuate these light signals, confining their polymerization potential to merely a few millimeters beneath the surface.
The Potential of Focused Ultrasound
Ultrasound presents a powerful alternative. With the ability to penetrate several centimeters into the body, focused ultrasound can effectively deliver heat to a specific targeted area without harming adjacent tissues. In 2023, researchers at Harvard University utilized this technique to activate polymerization by warming bio-inks made from poly(ethylene glycol) diacrylate. The drawback? The procedure necessitated temperatures ranging from 60–70°C—alarmingly high for use in living tissue.
As Stanford bioengineer Mark Skylar-Scott humorously remarked, this heating range is more akin to cooking meat than healing patients: “I don’t know about you, but I’d rather not be made medium rare.”
Thermal Sensitivity Breakthrough at Stanford
In a notable shift from previous techniques, a team led by Professor Wei Gao at Stanford University established a temperature-compatible protocol utilizing thermally sensitive liposomes—tiny spherical vesicles that dissolve or break open at body-safe temperatures (between 37°C and 42°C). These liposomes are pre-loaded with crosslinking agents and blended into thick injectable bio-inks along with ultrasound-sensitive contrast materials.
After injection, focused ultrasound selectively heats the liposomes at a determined internal location, starting the polymerization process. “These bio-inks are not akin to water—they’re thicker, making them unable to flow easily over a short time,” Gao explained. This targeted approach enables precise formation of materials where they are most needed within the body.
Multifunctional Polymer Fabrication
Using this strategy, Gao’s group successfully 3D printed an array of polymers inside living tissue. These included:
– Alginate hydrogels crosslinked with calcium chloride-loaded liposomes
– Free radical-cured polymers initiated by tetramethylethylenediamine
– Adhesive hydrogels crosslinked by sodium periodate capable of sealing internal injuries
Furthermore, the researchers augmented the functionality of these in-body printed substances by incorporating various agents. For example:
– Incorporating the chemotherapy medication doxorubicin led to a drug-releasing polymer. When positioned directly inside a mouse bladder near a tumor, the hydrogel localized treatment and significantly enhanced cancer cell mortality compared to standard drug delivery.
– Merging conductive nanomaterials like carbon nanotubes and silver nanowires resulted in electrically conductive polymers—offering promise for applications in implantable bioelectronic devices.
Safety and Bio-Clearance
Crucially, the ultrasound-activated process showcased a positive safety profile in both mice and rabbits. Injected bio-inks that did not undergo ultrasound-triggered polymerization were naturally eliminated from the body within seven days. Crosslinked structures, however, remained steady and intact—highlighting the accuracy and adaptability of the method.
Obstacles and Future Directions
Despite the exciting prospects of these advancements, challenges persist prior to clinical application. Gao’s team is currently concentrating on creating robust imaging and targeting algorithms capable of adapting to movement in dynamic tissues—such as the beating heart or expanding lungs. Real-time imaging integration will be vital to guaranteeing precision in these complex settings.
Mark Skylar-Scott, a tissue engineering specialist not linked to the study, lauded the innovation: “It’s an excellent advance in the field of in situ bio-printing.” He envisions that future versions could permit the sequential injection of different inks to design intricate, multi-material biological scaffolds directly within the human body. However, he notes that the current axial printing resolution is approximately 2mm—a detail he believes can and will be refined in forthcoming research.
Conclusion
Ultrasound-based in vivo 3D printing signifies a significant advancement in regenerative medicine and biomedical applications.