Overview of CRISPR
CRISPR is an innovative instrument that is reshaping lives and creating significant impacts in the healthcare sector. CRISPR, which stands for “Clustered Regularly Interspaced Short Palindromic Repeats,” is present in prokaryotes—tiny, single-celled organisms lacking organelles. These sequences reside within prokaryotic genomes, where a cell’s DNA is organized in clusters.
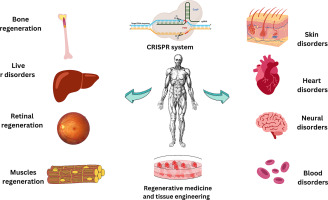
As a tool for gene modification, CRISPR is utilized to alter specific parts of DNA to address serious health conditions. It is particularly valuable because it aids the body in combating viral infections by assimilating the foreign DNA into its own genome, enabling recognition and destruction of the virus in future instances. Notably, in comparison to alternative gene-editing techniques, CRISPR is significantly more accurate and simpler to configure, allowing for a more straightforward redesigning of sequences. While other gene-editing tools generally depend on a single protein, CRISPR employs RNA-guided targeting combined with the Cas9 enzyme.
Mechanism of CRISPR
CRISPR operates by leveraging a natural defense strategy found in bacteria that enables them to detect and eliminate viral aggressors. When a virus infects a bacterial cell (a prokaryote), the bacteria incorporate a fragment of the invader’s DNA into their genome, serving as a genetic “memory.” This allows the bacteria to identify and react more efficiently to subsequent infections.
In the context of gene editing, this mechanism is modified using two essential elements: the Cas9 enzyme, which acts like molecular scissors to sever DNA, and guide RNA, which directs Cas9 to the precise genetic sequence requiring modification. After the desired DNA is cleaved, the cell’s natural repair processes engage, allowing researchers to implement changes to the genetic blueprint.
Unlike previous instruments that depended on difficult-to-reprogram proteins, CRISPR’s RNA-guided approach is more adaptable, simpler to create, and exceptionally precise. This ease and precision have enabled CRISPR’s implementation across medicine, agriculture, manufacturing, and microbiology—such as modifying microbes to boost product yields. However, as this article examines, the expanding capabilities also bring increasing ethical dilemmas, especially concerning germline modification and genetic enhancement.
The First Patient to Receive Personalized CRISPR Treatment
In February 2025, the first personalized CRISPR treatment was administered to a baby named KJ to address a deficiency in Carbamoyl Phosphate Synthetase 1 (CPS1)—an enzyme essential for converting ammonia (produced during protein metabolism) into urea. A team headed by Dr. Rebecca Ahrens-Nicklas and Dr. Kiran Musunuru at the Children’s Hospital of Philadelphia devised this treatment after extensive research in gene editing and collaborations with other healthcare professionals.
Their research concentrated on conditions affecting the urea cycle, which leads to harmful ammonia accumulation, resulting in harm to organs like the brain and liver. They customized the treatment specifically for KJ’s variant of CPS1 deficiency using preclinical data on similar cases.
So far, the only CRISPR therapies authorized by the U.S. FDA have been for more prevalent conditions such as sickle cell disease and beta thalassemia, impacting numerous patients. In KJ’s scenario, his treatment was conceptualized within six months of his birth, targeting his unique CPS1 variation. The team developed a base editing therapy carried via lipid nanoparticles to his liver to rectify the faulty enzyme.
The February treatment marked the first of three doses; KJ was given the subsequent doses in March and April 2025. Up until his final dose, he has not experienced any major side effects, demonstrates increased tolerance to dietary protein, and needs less medication to control ammonia levels. While continuous monitoring is necessary, Ahrens-Nicklas notes that the outcomes thus far are encouraging.
Ethical Implications of CRISPR
Like any pioneering technology, CRISPR invokes intricate ethical dilemmas. While its main aim is to modify somatic cells for disease treatment, it can also be applied to gametes, venturing into the contentious domain of germline editing. Changing DNA that will be passed on to future generations is frequently regarded as unethical—particularly when performed to enhance traits rather than cure diseases.
In light of these issues, researchers have temporarily halted germline editing until its ethical and