## Are Essential Oils Truly “The New Antibiotics?” An In-Depth Examination of the Assertions
Recently, essential oils and herbs have gained traction in mainstream culture, with claims of health advantages that range from enhancing mood to treating infections. Visit any ‘health food’ store or the herbal supplement section of your neighborhood supermarket, and you’ll encounter a variety of essential oils, herbal teas, and tinctures that tout potential health benefits. These items are frequently marketed as natural remedies that can alleviate a range of conditions, including bacterial infections. But how much of this is supported by robust scientific evidence versus mere exaggeration?
One notable example is an article in *The Atlantic* that recently caught my attention on social media. It examined the possibility that essential oils could act as new antibiotics, a concept that has undeniably piqued public interest. While it’s tempting to embrace the charm of natural remedies, several key scientific factors deserve scrutiny. Not all “bacteria-fighting” substances transition successfully from the lab to practical applications in human medicine.
### What Lies Beneath the Assertions?
The article put forth three primary arguments:
1. **Essential Oils in Livestock**: Essential oils, such as oregano oil, might serve as alternative treatments in livestock feed to lessen antibiotic use. Reducing antibiotic use in farming could, in effect, curb the emergence of antibiotic-resistant bacteria.
2. **Tea Tree Oil as a Disinfectant**: Tea tree oil has proven antiseptic qualities and is already included in many hand sanitizers and personal care items. This assertion is widely accepted, as tea tree oil is regularly utilized for its antimicrobial features in standard hygiene products.
3. **Essential Oils as Antibiotics for Humans**: Given that essential oils like oregano oil can eradicate bacteria in a lab setting, the article speculates they could potentially be used to treat infections in humans or animals. The author recommends further research but argues that the pharmaceutical sector has not pursued this avenue due to lack of financial incentive.
Among these three claims, the third prompts the most inquiry from a pharmacological viewpoint. The fact that oregano oil can eliminate bacteria in a petri dish does not equate to demonstrating that it can serve as an effective treatment for infections in humans. Here’s why the transition from lab results to practical application is considerably more complex than it appears.
### Why Bacteria Elimination in a Petri Dish Doesn’t Guarantee Efficacy in Humans
To grasp why essential oils are unlikely to be “the new antibiotics,” we must first reconsider what qualifies a substance as a useful pharmaceutical. Merely killing bacteria in a controlled laboratory setting (in vitro) does not inherently mean that it will be an effective treatment in living organisms (in vivo).
Let’s analyze this with established pharmacological principles.
#### 1. **Toxicity and Dosage Considerations**
A fundamental aspect of drug development is the appropriate dosage: for a drug to be effective, it must eradicate harmful microorganisms at concentrations considered safe. As toxicologist Paracelsus famously remarked, “The dose makes the poison.” A compound may be toxic to bacteria at elevated levels, but if that same concentration is also harmful to human cells, it won’t qualify as a viable medicinal option.
Even commonplace substances — like salt — can eliminate bacteria in a petri dish if used in sufficient quantities. The caveat is that the concentration required to kill bacteria could also be harmful to humans. Thus, the challenge lies not just in identifying compounds that can eliminate bacteria, but in locating those that do so at a “safe” level that remains non-harmful to humans.
### 2. **Understanding MIC**
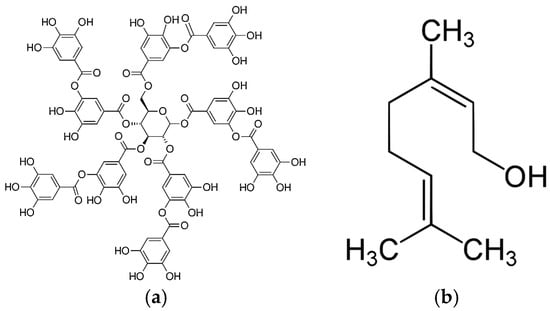
A crucial element in assessing whether a compound like carvacrol (an active constituent of oregano oil) might function as an effective antibiotic is its **Minimum Inhibitory Concentration (MIC)**: the lowest concentration of a substance needed to inhibit bacterial growth. A lower MIC indicates a more potent antibiotic, meaning only a small amount is required to eliminate bacteria.
For example, powerful antibiotics such as vancomycin possess low MIC values (typically in the realm of single-digit parts per million, ppm). Research indicates that the MIC of the active components in oregano oil, like thymol and carvacrol, are significantly higher, at around 140-175 ppm for certain bacterial strains. This highlights their relative weakness as antibiotics compared to established drugs like vancomycin, particularly against more resilient bacteria such as MRSA.
For clarity, when the MIC for a Staphylococcus strain concerning vancomycin exceeds 16 ppm, it is considered “vancomycin-resistant.” In contrast, thymol and carvacrol necessitate MICs close to 150 ppm, underscoring their comparative frailty.
### 3. **Chemical Stability and Solubility in Water**
For antibiotics to be effective, they must not only kill bacteria at low concentrations; they also need to remain in the body long enough to perform their function. This involves considerations of solubility, metabolism, and distribution throughout the organism. O