### Researchers Discover Breakthrough in Depression Treatment Via the Gut
For many years, medical professionals and researchers have explored innovative methods to tackle depression and anxiety—two of the most prevalent mental health issues globally. While traditional antidepressants have offered relief to millions, these treatments come with significant limitations, including unwanted side effects and safety concerns, especially concerning pregnant women. A recent revolutionary finding has shifted attention from the brain to the gut, presenting a hopeful new pathway for treatment that utilizes the body’s inherent gut-brain connection.
#### The Gut-Brain Connection: Beyond “Butterflies”
Many individuals instinctively recognize that emotions and the digestive system are linked. Nerves in your stomach may flutter when you’re anxious, and your appetite can disappear in times of sadness or stress. But what if this physical-emotional relationship could be leveraged to enhance mental health?
Research conducted by experts from Columbia University and NYU has shown that directing antidepressant medications specifically to the cells in the gut—rather than to the entire organism—could effectively address mood disorders like depression and anxiety, possibly with far fewer side effects. This study, published in the journal *Gastroenterology*, challenges traditional perspectives on how antidepressants function, introducing new possibilities for safer, more effective treatments.
“Serotonin has always been known to be involved in mood regulation,” states Dr. Mark Ansorge, an associate professor at Columbia University. “What we didn’t fully understand is how crucial the gut’s role is in this mechanism. By concentrating on intestinal cells, we might assist patients without the downsides of conventional antidepressants.”
—
#### Why the Gut? The Unexpected Role of Serotonin
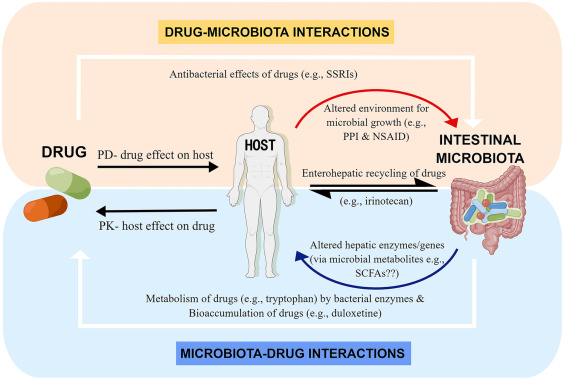
When individuals hear the word “serotonin,” they usually associate it with the brain. This chemical messenger is well-known for its importance in mood regulation, and most antidepressants, particularly SSRIs (Selective Serotonin Reuptake Inhibitors), aim to boost serotonin activity in the brain. However, what many fail to realize is that approximately **90% of the body’s serotonin is actually generated in the gut**, not the brain.
“Our gut’s serotonergic system greatly influences our brain function,” notes Dr. Kara Margolis, director of the NYU Pain Research Center. “It’s an enormous overlooked resource for creating innovative strategies for treating mental health disorders.”
Building on this understanding, the research team examined whether enhancing serotonin levels solely in the gut could lead to positive outcomes for mood and anxiety, while avoiding the adverse effects usually seen with systemic medications.
—
#### The Experiment: Assessing Gut-Directed Antidepressants in Mice
To validate their hypothesis, researchers employed advanced methods in genetic engineering, surgical procedures, and drug treatments. In a pivotal experiment, mice were genetically modified to exhibit increased serotonin signaling specifically in their gut, mimicking the effects of a gut-directed antidepressant. The results suggested that these mice demonstrated **decreased anxiety and depression-like behaviors** without experiencing the typical side effects associated with standard antidepressants, such as nausea or mental fog.
A significant revelation from this study was the involvement of the **vagus nerve**, a powerful nerve serving as a communication pathway between the gut and the brain. Although this nerve has been known for transmitting signals from the brain to the gut, the research discovered that signals propagating from the gut to the brain were vital to achieving the antidepressant effects observed in the mice.
—
#### Implications for Pregnant Women and Future Generations
Perhaps one of the most promising aspects of this research is its potential to refine treatments for pregnant women facing depression. While current antidepressants are effective, they have been shown to cross the placenta, possibly affecting fetal development. Observational data from this study indicated that children exposed to conventional antidepressants during gestation were three times more likely to develop gastrointestinal issues, such as chronic constipation, in their formative years.
The team does stress, however, that pregnant women currently on antidepressants should not discontinue their medication without consulting a healthcare provider, as the dangers of untreated depression during pregnancy—for both the mother and the child—can be severe.
“Our findings suggest that we can manage maternal depression or anxiety without endangering the developing fetus,” explains Dr. Ansorge. “This represents a crucial advancement toward offering safer treatment alternatives for pregnant patients.”
—
#### Looking Forward: The Promise of Gut-Targeted Antidepressants
Though it is still early in the research process, the teams at Columbia University and NYU are already pursuing the development of novel gut-targeted antidepressant medications based on their findings. These medications would aim to administer treatment via the digestive system, minimizing exposure to the rest of the body and lowering the chances of side effects.
If these efforts prove successful, this breakthrough could transform the approach to treating not just depression but also anxiety and related conditions. Individuals who have struggled to tolerate traditional antidepressants due to issues like brain fog, nausea, or fatigue may discover that gut-targeted therapies offer a more manageable and effective solution.
—
#### Wider Implications for