### Illuminating Cancer Cells’ Energy Sources: Pioneering Gene Therapy Concentrates on Mitochondria for Tumor Elimination
In the ongoing pursuit of cutting-edge cancer treatments, researchers are focusing on the cellular powerhouses – the mitochondria. Often called the “powerhouses” of the cell, these organelles are crucial for providing energy for a range of biological functions. For years, scientists have explored methods to hone in on mitochondria in cancer cells, acknowledging their essential part in the process of uncontrolled cell proliferation. However, a recent study from Ohio State University has made significant strides, introducing a gene therapy method that disrupts the internal workings of these energy sources, leading to extensive cancer cell death.
This innovative therapy utilizes nanoparticles that specifically target cancer cells, showcasing remarkable outcomes. In mouse models of glioblastoma, a highly aggressive brain cancer, and triple-negative breast cancer, significant tumor reductions and extended survival rates were observed, indicating potential for future human applications. This pioneering approach combines molecular biology with nanotechnology to precisely target cancer cells while sparing normal, healthy tissue.
### A Novel Approach: Focusing on the Mitochondrial Inner Membrane
For many years, mitochondria have been considered a promising target for cancer treatment studies. Mitochondria in cancer cells often exhibit heightened activity, catering to the energy requirements necessary for perpetual growth, division, and survival. The inner membrane of mitochondria is crucial for their energy generation – its impermeability and electrical charge differential make it a vital yet challenging target for intervention. However, five years ago, Dr. Zhou and his team found a way to take advantage of this vulnerability.
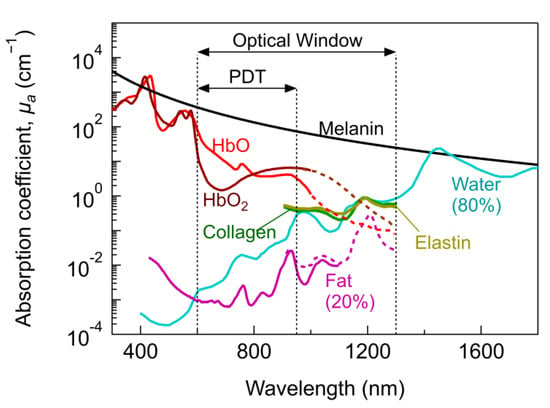
Zhou’s laboratory discovered that the inner membrane of mitochondria could be disrupted using proteins that create electrical currents. In previous tests, these proteins were stimulated with lasers to compromise mitochondrial structure and trigger cancer cell death. While encouraging, this method relied on external light activation, which created hurdles for clinical adoption.
The current study presents a novel method that allows light to be generated within cancer cells, negating the need for external laser stimulation and increasing the practical application of this technique in medicine.
### Mechanism of Action: Generating Light Inside Targeted Cancer Cells
The therapy features an advanced genetic delivery platform that combines two molecules: a light-sensitive protein known as **CoChR** and a bioluminescent enzyme. These components are carried within a modified adeno-associated virus (AAV), a non-harmful viral vector frequently used for gene delivery. When the virus reaches cancer cells, it initiates the expression of CoChR and the bioluminescent enzyme, which both localize within the mitochondria.
A distinct chemical injection activates the bioluminescent enzyme, prompting light production within the mitochondria of cancer cells. This internal illumination then activates CoChR, resulting in the creation of positively charged currents that disrupt the mitochondrial inner membrane. Consequently, this causes a catastrophic failure in the energy supply of the cancer cells – the mitochondria collapse, ceasing energy production and triggering widespread cancer cell death.
### Minimizing Side Effects: Guaranteeing Precision and Targeting
A vital component of the therapy is ensuring that normal, healthy cells are not affected. To accomplish this, the researchers incorporated various protective measures within their delivery system.
Dr. Liu’s team, specializing in targeted anti-cancer strategies, refined the specificity of the treatment by including a cancer-specific promoter protein in the AAV construct. This promoter guarantees that the genes for CoChR and the bioluminescent enzyme are expressed solely in cancer cells, leaving normal cells unaffected.
Furthermore, the AAV nanoparticle was encased in a natural nanocarrier derived from human cell lines. This design enhances the nanoparticle’s biocompatibility and stability within human biological fluids. The final phase includes attaching a monoclonal antibody to the particle, enabling it to identify specific receptors present on cancer cell surfaces. This highly focused approach allows the therapy to target malignant tissues while preserving healthy areas of the body.
### Encouraging Outcomes in Challenging Cancer Models
The treatment, known as **mLumiOpto**, was assessed in two notably difficult cancers: glioblastoma and triple-negative breast cancer. Glioblastoma, one of the most lethal brain cancer types, has very few treatment options and poor survival rates, whereas triple-negative breast cancer is an aggressive variant that does not respond to standard hormone receptor therapies.
In preclinical mouse studies, mLumiOpto demonstrated exceptional results. Tumors in treated mice were considerably smaller compared to those in untreated counterparts, and survival times notably increased in the glioblastoma cohort. Imaging studies further confirmed that the therapy was restricted to cancerous tissues, highlighting its high accuracy and minimal likelihood of off-target effects.
An additional promising finding from these studies was that the monoclonal antibody used to direct the therapy may also provoke an immune response against cancer cells present in the tumor microenvironment. If further