**A Revolutionary Method for Head and Neck Reconstruction Originates from Japan**
A remarkable surgical advancement has recently been presented by scientists in Japan, providing renewed optimism to patients confronted with the intricate challenges of complex head and neck reconstruction. This groundbreaking technique, created at Osaka Metropolitan University, is notable for its accuracy, safety, and versatility, broadening the spectrum of treatment alternatives for individuals who were previously deemed unsuitable for traditional reconstructive methods.
Head and neck reconstruction is vital for restoring both functionality and aesthetics in patients healing from trauma, disfiguring cancers, or extensive surgical procedures. It necessitates that surgeons carefully balance numerous priorities, including the preservation of essential functions such as speaking, eating, and breathing, alongside achieving a satisfactory cosmetic result. The method introduced by Dr. Tsubasa Kojima and his team is transforming the possibilities in this domain, offering solutions for situations once considered insurmountable.
—
### **The Limitations of Conventional Reconstruction**
Standard head and neck reconstruction generally utilizes *free flaps*. These are tissue sections that are completely separated from one area of the body and relocated to the reconstruction site, relying on being reattached to blood vessels through microsurgical techniques. Although often effective, free flaps may not be appropriate for everyone. Patients who have previously undergone radiation therapy, multiple surgeries, or those with compromised vascular health might not be able to tolerate this method.
Dr. Kojima, a lecturer at Osaka Metropolitan University’s Graduate School of Medicine, explains: “Traditional reconstruction typically employs free flaps, which may not be practical for some patients, especially those who have had previous radiation therapies or several surgeries.” These constraints leave numerous patients without feasible options, intensifying the emotional and physical challenges of their conditions.
—
### **The Breakthrough: Pedicled Latissimus Dorsi (LD) Myocutaneous Flaps**
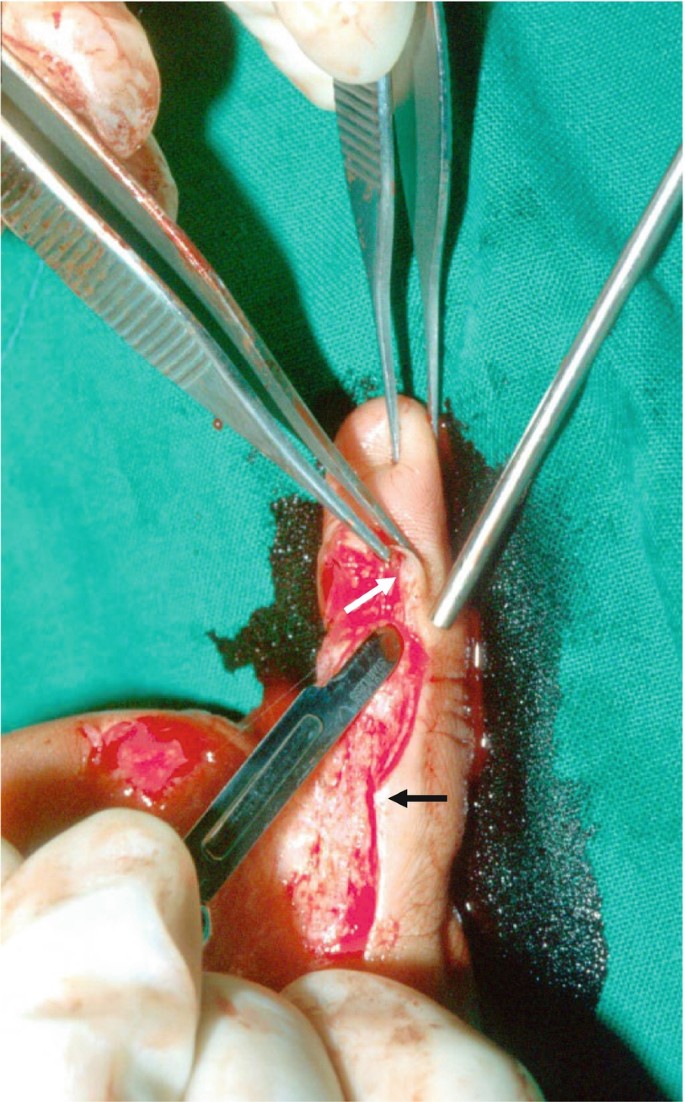
To tackle these challenges, the Osaka team has transformed the use of *pedicled flaps*, which differ from free flaps in that they are only partially detached from their donor site, thereby maintaining their natural blood supply.
The researchers utilized a technique featuring pedicled latissimus dorsi (LD) myocutaneous flaps—tissue segments taken from the back known for their reliability owing to their versatility and robust vascular supply. What distinguishes this method is a specific alteration: the skin segment of the flap is situated more distally (further down) on the back compared to traditional techniques. This modification permits the inclusion of a vital artery, the lateral cutaneous branch of the 10th posterior intercostal artery, ensuring consistent and strong blood circulation to the flap during and after its transfer.
—
### **Unprecedented Surgical Achievements**
In their clinical investigation, the team implemented this innovative pedicled LD flap approach on 22 patients with significant and intricate defects in the head and neck areas. Each procedure was executed flawlessly. This exceptional success rate carries significant implications for the domain of reconstructive surgery, particularly for patients with anatomical characteristics or medical histories that complicate conventional techniques.
“This configuration offers adaptability, enabling the LD flap to address large defects, including those in both the mouth and neck simultaneously, and even aids in jaw reconstruction by incorporating rib bone,” remarked Dr. Kojima. This dual capacity to address both soft tissue and structural bone deficiencies with precision and reliability highlights the innovation’s potential.
—
### **Broadening Surgical Possibilities**
The benefits of the pedicled LD flap technique are manifold. Firstly, its capability to integrate seamlessly into the diverse anatomical landscapes of the head and neck makes it adaptable to a broad array of defects. Secondly, it significantly minimizes the risks associated with free flap surgeries, especially for high-risk patients for whom free flap procedures might pose potential failures. For these patients, the pedicled flap provides not only a safer alternative but also a renewed chance at life.
Perhaps most notably, this method transforms the narrative for many patients traversing the challenging path of head and neck cancer recovery. By merging surgical accuracy with a focus on patient safety, the Osaka team’s approach fills voids in care, offering hope where options were once scarce or entirely absent.
—
### **A Major Advancement in Reconstructive Surgery**
The accomplishments of the Osaka Metropolitan University team signify more than just a technical advancement—it is a revolutionary change in how reconstructive surgeons tackle complex cases. With further validation and broader application, this innovation is set to become a fundamental element in the standard of care for intricate head and neck reconstruction globally.
For both patients and healthcare professionals, the results, as shared in *Plastic and Reconstructive Surgery—Global Open*, herald a more promising future—one where cutting-edge science harmonizes with compassionate care to restore not solely function but also dignity.
—
### **Glossary of Terms**
– **Free flap:** A section of tissue completely removed from one area of the body and reattached to blood vessels at the reconstruction site using microsurgical techniques.
– **Pedicled flap:** A section of tissue that retains its natural blood supply by remaining