**Historic Drop in US Obesity Rates: Analyzing the 2023 Milestone**
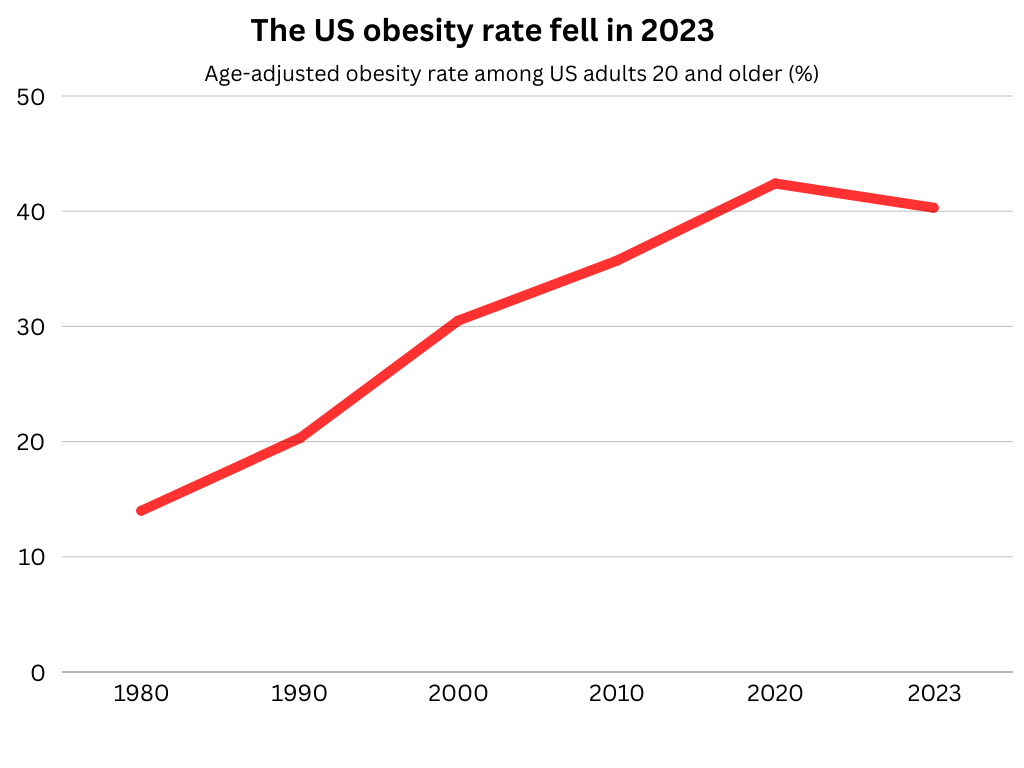
For the first time in more than a decade, the trend of obesity rates in the United States has taken a downward turn, signaling a hopeful advancement in the ongoing struggle against this public health challenge. According to pioneering research released in the *JAMA Health Forum*, obesity rates among adult Americans displayed a slight yet noteworthy decrease in 2023, following a decade of continuous increases that leveled off in 2022. This pivotal moment is linked to a combination of factors, including improvements in weight-loss medications and lifestyle changes associated with the COVID-19 pandemic.
—
### **Evaluating a Decade of BMI Trends**
The research, carried out by scholars from Boston Children’s Hospital and Harvard Medical School, offers a thorough examination of body mass index (BMI) and obesity trends from 2013 to 2023. The researchers analyzed a dataset encompassing over 47 million BMI readings, obtained from medical claims and electronic health records of more than 16 million US adults, to detect patterns in weight change across various years and demographics.
Results indicate that the average BMI within the population climbed steadily from 2013 to 2021, hitting a peak average BMI of 30.24 in 2021. This gradual rise abruptly stopped in 2022, with rates stabilizing before slightly decreasing in 2023 to an average BMI of 30.21. While the change may appear minor, it could signify the potential onset of a reversal in what had been an unyielding upward trajectory in obesity.
The medical sector is cautiously optimistic regarding this trend. Lead investigator Dr. Benjamin Rader from the Computational Epidemiology Lab at Boston Children’s Hospital stated, “Though the decline is modest, it represents a pivotal moment that might shape new approaches for tackling obesity in the years ahead.”
—
### **The Impact of Weight-Loss Medications**
A key factor contributing to this decrease seems to be the rising utilization of weight-loss medications, particularly GLP-1RAs (glucagon-like peptide 1 receptor agonists). Medications in this category, such as semaglutide, have shown impressive effectiveness in weight reduction during clinical trials. Initially intended for diabetes control, these drugs operate by regulating appetite and slowing down digestion, serving as a robust option for individuals dealing with obesity.
The study identified distinct regional disparities in the uptake of these medications, which appeared to align with obesity prevalence. The Southern US, traditionally home to the nation’s highest obesity rates, reported the most significant rate of GLP-1RA prescriptions, with 6.0% of patients receiving them, whereas the Western US recorded 3.4%. Simultaneously, the South experienced the most pronounced decline in obesity rates among all regions evaluated.
Nevertheless, researchers urge caution against oversimplifying the connection between medication usage and weight trends. Not every prescription equates to consistent or effective usage, and additional research is necessary to comprehend the broader implications of these medications on public health.
—
### **Changes in Social and Pandemic-Related Behaviors**
In addition to pharmaceutical solutions, changes in social behaviors during and post-COVID-19 may have influenced shifting weight trends. The pandemic prompted many to alter their lifestyles—both beneficial and detrimental—that could affect obesity rates:
– **Increased Health Awareness**: The pandemic illuminated health threats tied to obesity, such as a higher risk of mortality from COVID-19, prompting some to focus on weight loss and healthier practices.
– **Flexible Work Environments**: The emergence of remote work provided greater flexibility for meal preparation and integrating physical activities into daily life.
– **Stress and Economic Hardships**: On the flip side, ongoing stress and financial challenges may have intensified unhealthy eating habits for some individuals, a factor that future studies seek to investigate more thoroughly.
—
### **Demographic and Regional Insights**
The research indicated promising reductions in obesity rates among certain age and gender demographics. Adults aged 66 to 75 years observed the most significant drops in BMI, suggesting that older individuals might be taking advantage of superior medical innovations and improved access to preventive care. Additionally, women experienced greater reductions in rates compared to men, although the study has not yet determined the reasons for these gender-specific findings.
Regional patterns also drew interest. The South’s unique position as both a high-prevalence area for obesity and one of notable declines suggests that targeted interventions, such as increased access to medications, may be yielding results. However, researchers remind us that other factors specific to the South—like the disproportionately high COVID-19 mortality rates among those with obesity—could have influenced the 2023 results as well.
—
### **Study Limitations**
Although the outcomes are encouraging, several significant limitations must be acknowledged:
1. **Data Bias**: The dataset is based on medical records from healthcare visits, potentially leaving out individuals who are less active in the healthcare system.
2. **Medication Usage**: The study assesses the rates at which weight-loss drugs are dispensed but cannot confirm actual patient adherence or the effectiveness of treatment outcomes.