Title: Study from Finland Reveals Connection Between Early Antibiotic Use in Toddlers and Increased Childhood Obesity Risk
Recent research showcased at the Pediatric Academic Societies (PAS) Meeting in Honolulu reveals a notable association between antibiotic exposure in early life and a heightened risk of obesity among children. The study, derived from a thorough population analysis conducted in Finland, indicates that antibiotics given during the initial two years of life may have enduring consequences on a child’s body mass and general health.
Researchers at the University of Oulu in Finland utilized national health data to track 33,095 children born vaginally, examining their growth trends and medical backgrounds. The findings were striking: children who were administered antibiotics in their first two years showed elevated body mass index (BMI) scores and had a 20% increased likelihood of becoming obese by age 12 compared to their counterparts who did not receive antibiotics during this period.
Key Developmental Phase
Dr. Sofia Ainonen, the principal investigator and medical expert at the University of Oulu, emphasized the importance of the timing of antibiotic exposure. The research team evaluated various developmental phases, including maternal antibiotic use before and during pregnancy, alongside perinatal exposure, but concluded that only the first two years post-birth had a significant correlation with later obesity.
“Antibiotic administration during the first two years of life is more closely linked to childhood weight gain compared to exposure at pregnancy stages or other early years,” stated Dr. Ainonen.
Data from the study illustrated that toddlers who were prescribed antibiotics experienced an adjusted BMI increase of 0.067 (taking sex and age into account), a minor-seeming figure that equated to a 9% higher risk of being overweight and a 20% escalation in obesity risk by the time they reached school age.
Prevalent Exposure
One of the most striking elements of the study was the high prevalence of early antibiotic exposure among participants. A substantial 68% of the children had received antibiotics within their first two years, amplifying the need to comprehend the far-reaching effects of this standard medical practice.
In contrast, only 27% of the corresponding mothers were administered antibiotics during pregnancy, and 21% of children faced exposure in the perinatal phase. Notably, neither of these exposures displayed a significant link to changes in childhood weight, thereby underscoring early childhood as a crucial period of concern.
Concerning Obesity Trends
With over 159 million school-aged children globally classified as obese in 2022, this study contributes to the expanding pool of research aimed at understanding the factors influencing this worldwide health issue. Recognizing adjustable risks such as the use of medications during infancy could be crucial for addressing this increasing concern.
Earlier studies have already highlighted early-life antibiotic usage as a factor in various health outcomes, ranging from a greater allergy risk to hindered immune system development. This research provides compelling evidence that weight regulation may also be influenced, spotlighting the enduring metabolic effects of disrupting initial gut health.
Microbiome Disturbance: The Possible Mechanism?
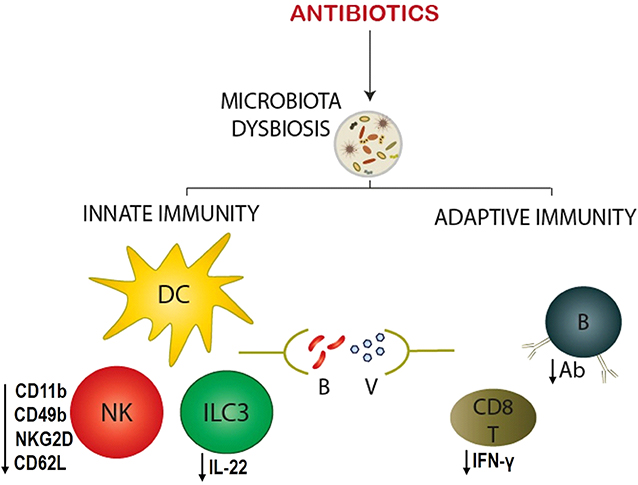
The gut microbiome—a complex ecosystem of microorganisms essential for digestion, immunity, and metabolic balance—has come under increasing scrutiny regarding its impact on health outcomes from infancy onward. Antibiotics are known to significantly modify the microbiome’s composition, particularly when given during its early developmental stages.
Dr. Ainonen and her research group propose that altering the microbiome at such a crucial time may disrupt the body’s capacity to regulate weight effectively over the long haul. Evidence suggests that shifts in microbial diversity during infancy can affect fat storage, appetite control, and insulin sensitivity—all factors that can lead to weight gain.
Clinical and Public Health Considerations
These results pose significant questions regarding antibiotic management in pediatric care. Although antibiotics can be essential, their excessive use—especially for viral infections like colds and flu, where they are ineffective—may result in unintentional long-term effects.
“Healthcare providers must exercise caution when prescribing antibiotics to young toddlers, particularly unnecessary ones for upper respiratory infections,” Dr. Ainonen stressed.
This prudence is especially warranted when symptomatic treatment or monitoring could serve as reasonable alternatives to prompt antibiotic intervention.
Looking Forward
The research team intends to explore more deeply the biological and molecular mechanisms that could link early antibiotic use with childhood obesity. “Future research focusing on the potential causal relationships between early-life antibiotics and child overweight and obesity should emphasize antibiotics used in the first two years,” concluded Dr. Ainonen.
These findings underscore the importance for both parents and healthcare professionals to contemplate the long-term consequences of early medical treatments. With global rates of pediatric obesity continuing to soar, preventive strategies—especially those addressing alterable early-life exposures—are vital.
Conclusion
The Finnish study acts as a crucial call to action for healthcare providers, underlining the necessity for careful antibiotic usage during a child’s formative years. Decisions made during this pivotal period could significantly influence a child’s lifelong health trajectory, particularly in fighting the rampant issue of childhood obesity.
As research progresses, a better understanding of the gut microbiome and its