Unlocking the Mind: A Revolutionary Non-Invasive Neural Interface Innovation in Spinal Cord Injury Rehabilitation
In an extraordinary development, researchers at Washington University in St. Louis have created an innovative non-invasive neural decoder that could transform the rehabilitation and treatment of spinal cord injuries (SCI). By establishing a direct link between the brain and spinal cord, this technology has the potential to improve mobility recovery in ways that were once deemed impossible without surgical procedures.
A Brain-Computer-Spine Connection — No Surgery Needed
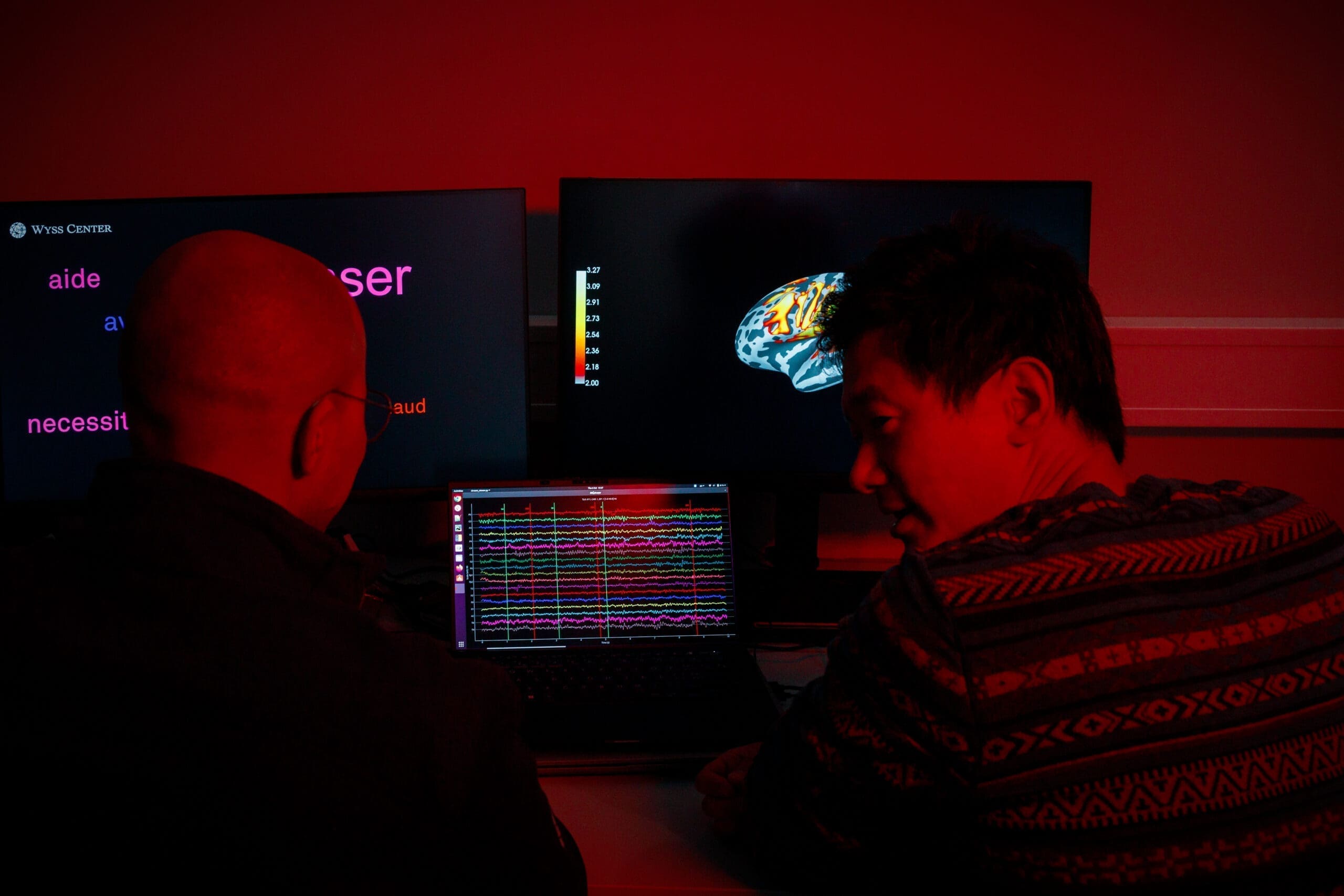
The team, overseen by Ismael Seáñez, assistant professor of biomedical engineering at WashU, has successfully showcased a prototype system that interprets brain activity through electroencephalography (EEG) and subsequently administers synchronized electrical stimulation to the spinal cord. In contrast to traditional methods that necessitate implanted electrodes, this system is completely non-invasive. The results were recently published in the Journal of NeuroEngineering and Rehabilitation.
“When an individual experiences a spinal cord injury, the brain is still capable of generating the command to move, and the spinal circuits below the injury can still receive instructions—but the connection is severed,” Seáñez stated. “Our objective is to bridge that divide by decoding the brain’s intention and directly stimulating the spinal cord.”
Understanding the Mechanism
The procedure initiates with a participant donning an EEG cap equipped with surface electrodes that capture electrical activity from the brain. The participant is instructed to either execute a physical movement (like extending the knee) or simply envision doing so. During these activities, the EEG gathers brainwave data, specifically tracking changes known as “event-related desynchronization” — patterns that manifest when the brain gears up to move.
This information is then processed with a Linear Discriminant Analysis (LDA) algorithm — a machine learning model selected for its straightforwardness and effectiveness. The algorithm adeptly learns to recognize the brain’s motion intent and signals a device to deliver electrical stimulation to the spinal cord through the skin, facilitating movement in the corresponding muscle group.
The outcomes were striking: the system attained 83% accuracy in identifying actual movement intent and 77% accuracy when participants merely imagined moving — a vital feature for people with complete paralysis.
A Crucial Advancement for Recovery and Neural Rehabilitation
For those living with spinal cord injuries, rehabilitation often stagnates after six months due to limited interaction between the brain and the damaged spinal cord. This innovation presents the possibility of extending—and enhancing—recovery by re-engaging spinal circuits utilizing the brain’s own electrical signals, even years post-injury.
Current intensive rehabilitation efforts usually involve physical therapy and robotic devices, yielding mixed outcomes. Since the WashU system relies solely on external devices, it sidesteps the complications and expenses linked to surgical implants, rendering it a compelling option for wider clinical application.
Challenges in Real-World Application and Future Development
Despite the encouraging data, numerous challenges persist. Notably, the decoder currently delivers optimal performance with cued movements, where participants are responding to prompts. The system proves less reliable with self-initiated or spontaneous movements, likely due to slight variations in brain signal patterns.
The research team is investigating methods to generalize their decoder so it can learn from data across various subjects. This would streamline clinical deployment by minimizing the need for individual calibration, which can be time-consuming and technologically intricate. Additionally, there is interest in refining the system for better functionality in real-life, uncontrolled settings.
Broad Clinical and Economic Consequences
With approximately 18,000 new spinal cord injury cases each year in the United States and rehabilitation expenses exceeding $500,000 in the first year following injury, the need for affordable and effective recovery solutions is substantial. A non-invasive, wearable brain-computer-spine interface could significantly transform the existing treatment landscape, offering a scalable and safer alternative to invasive neurosurgical procedures.
For the expanding neurotechnology sector, this represents a potential shift. While considerable venture capital has flowed into implant-based systems (such as Neuralink or BrainGate), the success of external solutions might lower adoption barriers and enhance accessibility.
Regulatory and Policy Considerations
As brain-computer interface (BCI) technology progresses, regulatory frameworks must adapt. Non-invasive systems challenge the distinctions among medical devices, consumer technology, and neurotherapeutics. Policymakers may need to create new standards and guidelines to ensure safety, efficacy, and equitable access while promoting innovation.
From Research to Real-World Application
The investigation received funding from the McDonnell Center for Systems Neuroscience, the National Institutes of Health, and various departments at Washington University. Although currently in initial evaluation stages, the research team is hopeful about advancing toward clinical trials.
“What we’ve accomplished is decoding the intention to move,” Seáñez remarked. “This can serve as the groundwork for a wearable system that doesn’t necessitate surgery. If we can instruct it to respond to imagined movements, even patients with complete paralysis could regain some control over their own bodies.”
The Road Ahead
Further studies will be required to optimize the system for immediate, practical use.