Microscopic ‘Cellbots’ Present Major Advancement in Precision Stem Cell Therapy for Brain Disorders
In a pioneering development that could fundamentally transform the treatment landscape for brain disorders, researchers have created microscopic robots adept at delivering stem cells precisely to specific brain regions and triggering their conversion into functional neurons. This innovative approach has the potential to change the course of regenerative treatments for neurodegenerative diseases, including Parkinson’s disease, Alzheimer’s disease, and brain injuries resulting from strokes.
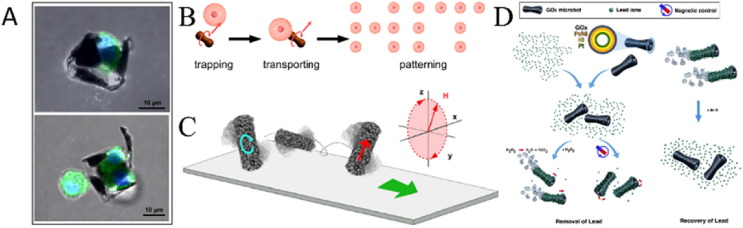
Recent findings published in Microsystems & Nanoengineering unveil the emergence of “Cellbots”—a unique combination of human neuroblastoma cells and magnetic nanoparticles. These minuscule, programmable entities function like tiny couriers, stealthily traversing the complex terrain of brain tissue through external magnetic fields while carrying the biochemical essence of stem cells.
A Dual-Innovation Approach
The new technology targets two of the most significant obstacles in neural stem cell treatment: precise delivery and targeted activation. Historically, stem cell therapies for neurodegenerative conditions have encountered substantial challenges. Upon injection, the cells often disperse unpredictably or struggle to integrate appropriately into damaged neural pathways. Additionally, without accurate control, the stem cells may not differentiate into the specific types of functional neurons needed for effective treatment, consequently diminishing treatment outcomes.
Under the leadership of Dr. Hongsoo Choi from the Daegu Gyeongbuk Institute of Science and Technology in South Korea, researchers have effectively combined magnetic navigation and micro-ultrasound technology to address both issues concurrently.
“By integrating the precision of magnetic actuation with the non-invasive influence of ultrasound, we’ve designed a scalable platform for neural regeneration,” Dr. Choi stated.
Ultrasound-Activated Neuron Development
After the Cellbots reach their designated spot in the brain, a specially designed piezoelectric micromachined ultrasound transducer (pMUT) directs targeted sound waves to activate the stem cells. Unlike traditional therapeutic ultrasound tools, the pMUT used here is extremely miniaturized—merely 1 millimeter wide and 7 millimeters long, with each element measuring just 60 micrometers in diameter, which is slightly smaller than a human hair. This level of precision ensures targeted stimulation without affecting surrounding healthy tissues.
Laboratory experiments yielded remarkable outcomes: 40 minutes of ultrasound exposure led the stem cells to develop neural extensions nearly double the length of those in control groups. This significant increase in neural projections indicates strong stimulation of differentiation, suggesting the stem cells were effectively progressing into neurons.
Magnetically Controlled Microbots Demonstrate Surgical Accuracy
The Cellbots are navigated through soft tissues with micrometer-level precision utilizing external magnetic fields. This precise control empowers scientists to direct the stem cells through intricate neural networks to specific locations, such as areas impacted by Parkinson’s disease. The combination of delivery accuracy and targeted ultrasound stimulation ensures that only the desired cell clusters are activated, minimizing the risk of unwanted effects and unintended cellular growth.
“Achieving localized differentiation paves the way for therapies where stem cells can be delivered precisely to areas affected by disease and encouraged to mature into the types of cells lost in neurodegenerative ailments,” Dr. Choi remarked.
Prospects for Neurodegenerative Disorders and Beyond
This advancement holds considerable promise for conditions like Parkinson’s disease, characterized by the loss of dopaminergic neurons in a specific brain area. With Cellbots, healthcare providers might eventually be able to deliver stem cells straight to that area and promote their development into healthy dopamine-producing neurons, potentially restoring normal brain function.
Additionally, the technology carries broader implications beyond neurodegenerative diseases like Parkinson’s and Alzheimer’s. Stroke survivors may experience localized brain tissue restoration, and the precision of this method may facilitate the creation of laboratory-based neural models for drug testing, enhancing the validity of experimental treatments prior to human trials.
Awaiting Human Trials
Despite the revolutionary nature of this approach, it has yet to be tested in live animals or humans. The research remains in the preclinical phase, with ongoing endeavors to refine the ultrasound parameters and expand the technology for wider medical application.
Nevertheless, the success of these preliminary studies signifies a significant stride in neural engineering. By overcoming essential limitations in stem cell therapy, the Cellbot platform provides a promising avenue toward new, less invasive solutions for the millions affected by untreatable brain disorders.
A Vision for the Future of Medicine
With ongoing advancements, the combination of microrobotics and bioengineering could herald a new era in which damaged brain circuits are repaired with remarkable precision—microscopically, non-invasively, and on demand.
In closing, Dr. Choi noted: “This is merely the beginning. The tools we’ve developed could ultimately make regenerative medicine more predictable, personalized, and potent than ever before.”
To stay informed about such advancements—and to support independent, trustworthy science journalism—consider contributing to platforms that link readers with the stories that will shape the future.