It all started as a note hidden within hospital documentation: cancer patients who received a COVID-19 mRNA vaccine shortly after commencing their immunotherapy experienced significantly longer lives. Much longer. What initially appeared to be a mere coincidence now seems to signal a breakthrough that could change how medicine engages the immune system in combating cancer.
Investigators from the University of Florida and the University of Texas MD Anderson Cancer Center examined data from over 1,000 individuals with advanced lung or skin cancer. Those who were administered a COVID-19 mRNA vaccine within 100 days of initiating immunotherapy drugs showed markedly improved survival rates compared to those who were not vaccinated. The findings, shared this week at the European Society for Medical Oncology Congress in Berlin, imply that mRNA vaccines may contribute more than just infection prevention. They could potentially “activate” the immune system to confront tumors.
The Unintentional Cancer Tool
For UF pediatric oncologist Elias Sayour, M.D., Ph.D., this discovery represents the pinnacle of nearly ten years of inquiry into how mRNA can invigorate the immune system. His laboratory had previously demonstrated that a nonspecific mRNA vaccine, which does not target a specific virus or cancer, could provoke a strong antitumor response in mice. This revelation raised a compelling question: could the COVID-19 vaccine have comparable impacts on humans?
“The ramifications are extraordinary — this could transform the entire landscape of oncologic treatment,” remarked Sayour. “We might be able to develop an even more effective nonspecific vaccine to activate and reset the immune response, potentially creating a universal, readily available cancer vaccine for all patients.”
When Sayour’s former student and present MD Anderson oncologist Adam Grippin, M.D., Ph.D., examined clinical records, the trend was remarkable. Among patients diagnosed with Stage 3 and 4 non-small cell lung cancer, those who obtained a COVID vaccine around the initiation of immunotherapy had a median survival of 37.3 months—compared to just 20.6 months for those who did not receive the vaccine. In cases of metastatic melanoma, survival increased from 26.7 months to as high as 40 months. Vaccinations for flu and pneumonia provided no such advantage.
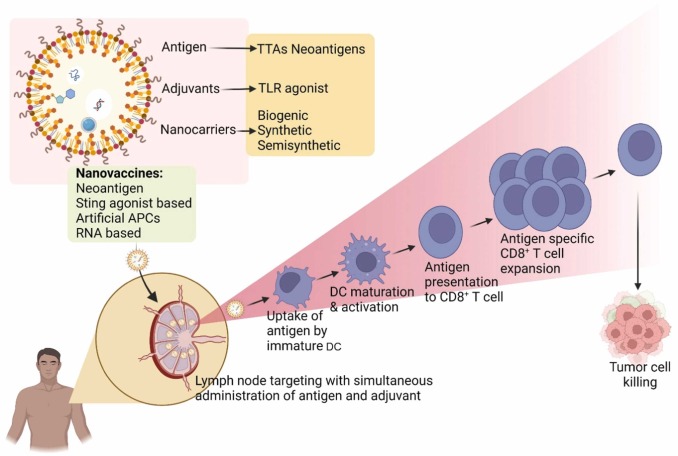
In mouse studies, coupling immunotherapy with an mRNA vaccine aimed at the coronavirus spike protein also transformed previously non-responsive tumors into responsive ones. “One of the mechanisms behind this effect is that administering an mRNA vaccine acts like a signal that mobilizes immune cells from unproductive areas like tumors to beneficial sites such as lymph nodes,” Sayour elucidated.
Changing the Landscape of Immunotherapy
External experts advise that these findings could herald the beginning of a novel strategy in cancer treatment. Jeff Coller, Ph.D., an mRNA researcher at Johns Hopkins University, referred to the findings as another surprising legacy of Operation Warp Speed, the U.S. government’s early pandemic effort to hasten vaccine creation.
“The findings from this study illustrate how potent mRNA therapies are and that they are transforming our approach to cancer treatment,” stated Coller.
Nevertheless, the researchers urge caution, noting that the data are observational. A large, randomized clinical trial is already in the works through the UF-led OneFlorida+ Clinical Research Network, which includes hospitals and clinics across six states. If confirmed, the vaccine’s non-specific immune activation could signify a new therapeutic frontier—one that enhances existing checkpoint inhibitors without causing additional toxicity.
Duane Mitchell, M.D., Ph.D., director of the UF Clinical and Translational Science Institute, stated that the magnitude of the effect is notable even by oncology standards. “While not yet proven to be causal, this represents the kind of treatment advantage we aspire to and hope to achieve with therapeutic interventions—but seldom do,” he expressed.
As the data await validation, Sayour’s team is already preparing next-generation mRNA constructs specifically designed to reset immune responsiveness across various cancers. For patients facing advanced-stage illness, even a slight prolongation of life could distinguish between running out of time and gaining more of it.
Reports and Proceedings: 10.1016/j.esmo.2025.10.001
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort,