**Innovative Injectable Treatment Seeks to Alleviate Post-Stroke Brain Injury**
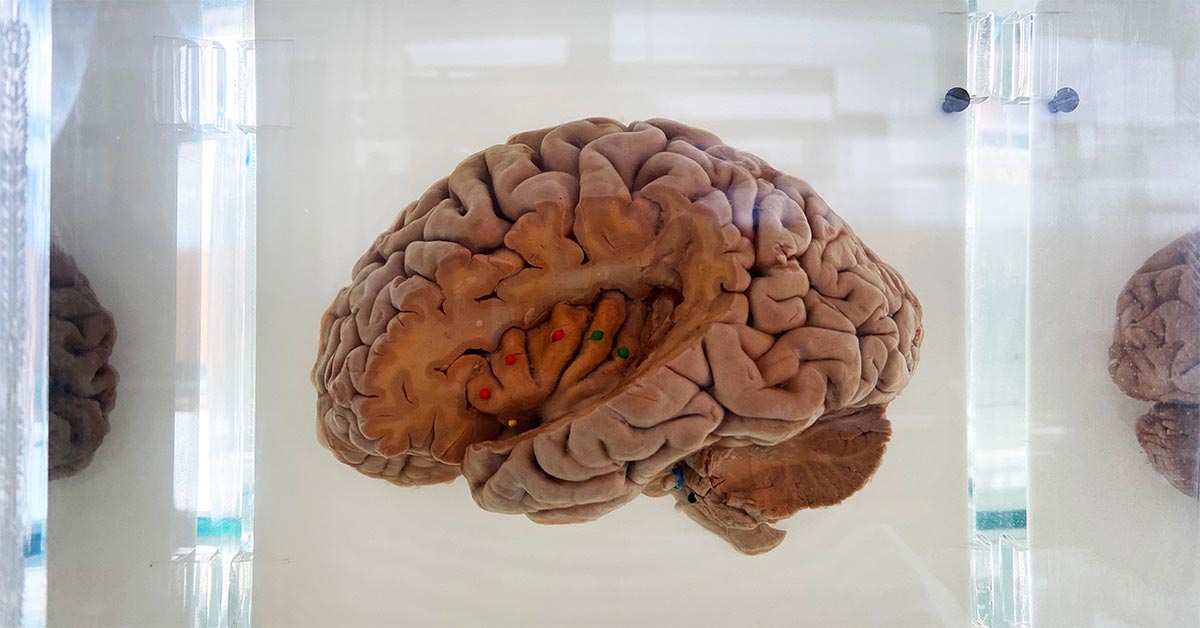
Strokes continue to be a primary cause of mortality and disability globally, with ischemic strokes making up about 80% of cases. Although medical innovations have greatly enhanced the capability to swiftly eliminate blood clots and restore blood flow, this often gives rise to a secondary risk termed ischemia-reperfusion injury. This critical condition arises when the abrupt resumption of blood flow initiates inflammation and cell death as the brain’s immune response reacts destructively to previously oxygen-deprived tissues.
Researchers from Northwestern University are forging ahead with a novel solution to this challenge using injectable ‘dancing molecules.’ These engineered peptide formations are distinguished by their perpetual movement, enabling them to navigate past the blood-brain barrier and specifically target the affected areas of the brain. In recent trials involving mice, a single intravenous administration of these peptides immediately following the restoration of blood flow effectively curtailed brain damage. This promising strategy emphasizes not only the restoration of blood flow—which is the main focus of existing stroke treatment protocols—but also the reduction of inflammatory responses and cell death subsequent to reperfusion.
The mechanism of the peptide therapy utilizes advanced supramolecular techniques, where the peptides remain small during circulation but expand into larger complexes upon reaching damaged regions. This is especially advantageous in addressing stroke-related injuries, as the peptide assemblies have been shown to concentrate in the ischemic hemisphere of the brain—a zone where the blood-brain barrier temporarily becomes more permeable following a stroke event.
In controlled studies, mice treated with peptides exhibited smaller infarcts and diminished inflammation in comparison to untreated counterparts over a week-long period. Furthermore, these peptides showed biocompatibility, with no signs of organ damage or immune rejection observed in the treated mice. This points to a promising possibility for the safe translation of the therapy into human use, although additional studies are essential to further validate these results.
The initiative holds potential beyond stroke management. The versatile peptides operate not as fixed entities but as signals that promote interaction with cellular receptors essential for survival and repair. This adaptability opens doors for therapeutic applications in traumatic brain injuries or even neurodegenerative conditions like ALS.
While no immediate behavioral enhancements were detected in the treated mice, the decrease in tissue damage suggests the likelihood of improved long-term neurological recovery outcomes. Ongoing investigations will delve into this potential and assess whether incorporating regenerative signals could amplify the therapeutic efficacy of the peptides.
In summary, this research represents a significant shift in stroke care methodology, broadening the focus from simply clearing clots to mitigating inflammation and fostering neural recovery mechanisms. The findings are documented in the journal Neurotherapeutics, promoting wider accessibility and inspiring further contributions to advancements in stroke medicine.