IT IS a biological stowaway that nearly every adult on the planet harbors, a silent companion nestled within the very immune cells designed to guard us. For many, the Epstein-Barr virus (EBV) is a benign squatter, a remnant of a childhood fever or a teenage episode of glandular fever that has entered a lifelong dormancy.
However, in some cases, the companion awakens. And when it does, the effects can be catastrophic, ranging from multiple sclerosis (MS) to Hodgkin’s lymphoma. Until now, monitoring this unseen battle between host and virus in healthy individuals was nearly impossible. We acknowledged the virus’s presence, but we couldn’t observe how diligently the body was laboring to keep it subdued.
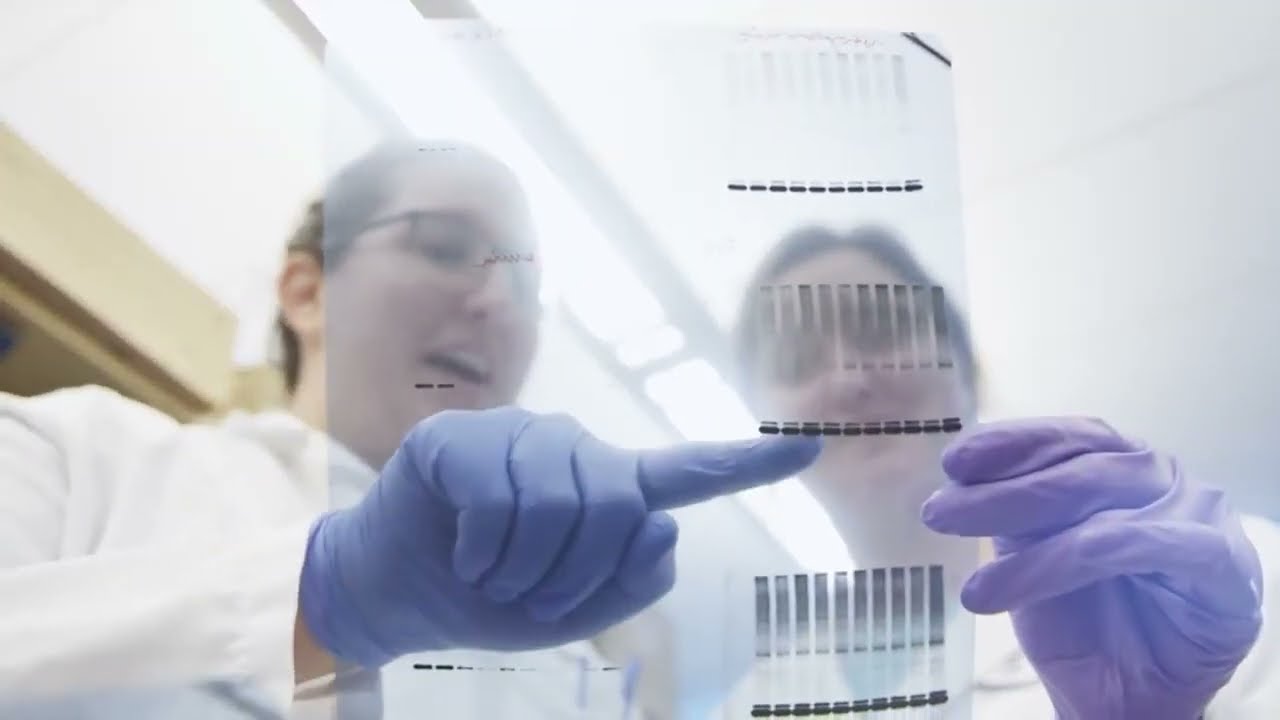
“In spite of its significant relevance, very little understanding exists regarding how precisely the immune system manages chronic EBV infection,” states Kerstin Ludwig at the University Hospital Bonn in Germany. She clarifies that the issue has always been a deficiency of data. Assessing the “viral load”—the quantity of virus actively circulating—necessitates specific, costly laboratory tests that simply aren’t carried out on hundreds of thousands of healthy individuals.
Recently, Ludwig and her colleague Axel Schmidt discovered a method to “repurpose” one of the most extensive collections of biological data in history to reveal the virus’s concealed locations. By analyzing the genetic sequences of nearly 800,000 participants from the UK Biobank and the US-based All of Us project, they have pinpointed the genetic and lifestyle elements that determine who maintains control over the virus and who allows it to break free.
The breakthrough emerged from examining what most geneticists consider “noise.” When researchers sequence a human genome, they aren’t merely capturing human DNA; they are also gathering fragments of everything within that person’s blood at the time. “Genome sequencing data is actually collected to characterize the human genome—so we have ‘repurposed’ it somewhat,” explains Schmidt.
By searching for brief fragments of DNA that corresponded to the EBV genome rather than the human one, the team was able to estimate the viral load in each individual. They detected these viral “reads” in approximately 16 to 22 percent of the subjects analyzed. Those with the highest levels of viral fragments weren’t just unfortunate; they exhibited specific characteristics that indicated their immune systems were under pressure.
One of the most notable observations was the association with smoking. It has long been acknowledged that smoking is a risk factor for EBV-related diseases, but the “why” has remained elusive. Schmidt’s data suggests a direct correlation: “Our data indicate that current smoking, in particular, elevates EBV viral load.” It appears that the chemical barrage of a cigarette does not solely harm the lungs; it may impair the innate immune system’s capacity to keep EBV in its dormant state.
The team also observed a seasonal pattern in the virus. Samples collected during the winter months tended to show higher viral loads compared to those gathered in the summer. This finding hints at the subtle ways our environment—possibly through vitamin D levels or the stress of winter illnesses—tilts the balance in favor of the virus.
But the true treasure was embedded within the DNA itself. The researchers identified 27 areas of the human genome, outside the well-established immune system centers, that appear to influence EBV regulation. Some of these genes are already recognized to cause rare, severe immune deficiencies when they malfunction, but Schmidt and Ludwig discovered that common variations in these same genes can impact how effectively a “healthy” individual manages their viral stowaway.
This isn’t merely an issue of intellectual curiosity. By comparing these genetic “control” regions with the DNA profiles of different diseases, the team found significant overlaps. They uncovered that the same genetic variants that hinder the body’s ability to regulate EBV are also related to an increased likelihood of multiple sclerosis and rheumatoid arthritis. In the case of MS, a particular immune-tagging gene known as *HLA-A*02:01* emerged as a key regulator, aiding the body in maintaining better control of the virus and consequently reducing disease risk.
Perhaps most unexpectedly, the study suggested that EBV plays a role in conditions where it was never previously anticipated, such as type 1 diabetes.
“Our findings provide a foundation for comprehending EBV immunity,” says Ludwig. By transforming the by-products of genomic research into a diagnostic tool, the team has not only illuminated one virus. They’ve laid the groundwork for monitoring other “silent” infections that may be shaping our health from the background. For the 95 percent of us who bear EBV, the stowaway may still be present, but it is finally beginning to shed its cloak of anonymity.
Study link: <a href="https://www.nature.com/articles/s41586-