A single drop of blood could soon be all that’s needed to perform a wide range of health tests. Researchers at Stanford University have been using mass spectroscopy to determine the levels of key chemicals in tiny volumes of blood.
Although the approach sounds similar to the fake technology touted by the fraudulent US biotech firm Theranos, which collapsed in 2018, the researchers’ peer-reviewed study describes how their method works – something Theranos never did.
‘Our goal is to measure lots of analytes in blood – that part’s the same,’ says Michael Snyder, director of Stanford’s Center for Genomic and Personalized Medicine. ‘And the kinds of molecules we’re doing overlap [with Theranos] but they’re different.’
While Theranos claimed they were using established diagnostic procedures to monitor health from a single drop of blood – an approach that proved impossible – Snyder’s team are using mass spectroscopy to analyse the levels of more than 2000 proteins, lipids and metabolites in the blood.
Theranos also falsely claimed to have combined all its tests in a single device, but it takes Snyder’s team about a day in a laboratory to complete an analysis.
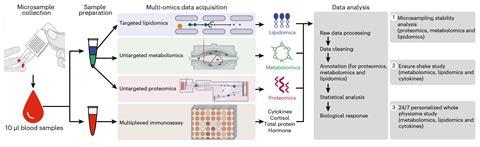
Using just 10µm of blood (a ‘drop’ is about 50µm) the team was able to determine levels of 128 proteins, 1461 metabolites and 776 lipids. A second 10µm sample was used to measure inflammatory markers, and they were combined in an approach called ‘multi-omics’ to create a comprehensive chemical profile.
Many of the results were comparable to standard diagnostic tests – the level of the stress hormone cortisol, for example – but not every chemical in blood is a signal of health, Snyder says.
Among other applications, the research used the approach to study reactions to the consumption of a ‘shake’ containing carbohydrates, fats, proteins and micronutrients. The team found that the shake provoked a very different set of responses in different people. The team also used it to monitor how the blood levels of cortisol and glucose varied in a volunteer – Snyder, in this case – over the course of a day.
Snyder says this approach can help monitor the chemical responses of individuals in a variety of circumstances, and the next step will be to apply it to a broad group of patients in pilot studies.
Bioinformatician Christoph Bock, the principal investigator at the Research Center for Molecular Medicine (CeMM) in Vienna, points out that blood ‘microsampling’ for glucose has proven useful in diabetes care. However, he cautions it may not be able to replace standard laboratory tests due to technical challenges, and because capillary blood sampled in a drop from a finger might not accurately reflect the blood’s full molecular profile.
But he sees promise in the approach. ‘I personally see the most interesting aspect of this study in the integration with wearable sensor data ,’ he says, noting that it might become possible to link patterns detected non-invasively by wearables to the molecular changes detected by microsampling.