Waist-to-Height Ratio Proves to Be a More Reliable Indicator for Heart Failure Than BMI, Recent Research Shows
A pioneering study set to be showcased at the upcoming Heart Failure 2025 congress, organized by the European Society of Cardiology (ESC), has found that waist-to-height ratio serves as a more reliable indicator of heart failure risk compared to the traditionally used Body Mass Index (BMI). Research conducted by scientists at Lund University in Sweden emphasizes that fat distribution, especially in the abdominal area, is crucial to cardiovascular health outcomes, more so than previously recognized.
Rethinking BMI: Moving Beyond a Conventional Metric
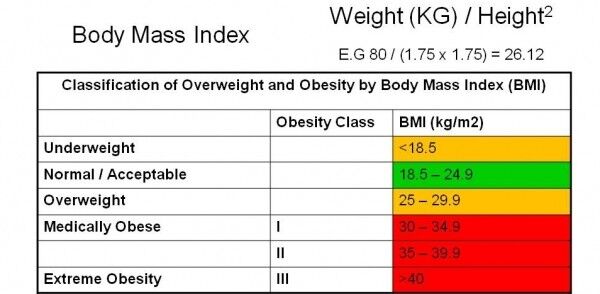
For numerous years, BMI has been regarded as the essential clinical measure to evaluate weight-related health risks. BMI is calculated by dividing weight in kilograms by the square of height in meters, but it fails to distinguish between muscle and fat and does not consider fat distribution. Consequently, it may miss individuals whose risk of disease arises from abdominal fat, despite fitting within a “healthy” weight category.
“BMI varies with sex, ethnicity, and other personal factors and it does not reflect the harmful buildup of fat around vital organs,” stated Dr. Amra Jujic from Lund University during her presentation. “The waist-to-height ratio presents a clearer picture by emphasizing central adiposity, which is more metabolically active and harmful.”
Grasping the Concept of Central Adiposity
Central adiposity refers to fat accumulating around the belly and internal organs, like the liver and pancreas—this type of fat is linked with chronic inflammation, insulin resistance, and cardiovascular disease. Researchers are increasingly pinpointing this specific fat distribution as a significant risk factor for heart-related conditions, even in individuals classified as having a normal weight by BMI standards.
The Malmö Preventive Project: An Extensive Long-Term Study
To explore this correlation, the research team at Lund University monitored 1,792 participants aged between 45 and 73 from the Malmö Preventive Project over an average duration of 12.6 years. The study group was meticulously selected to achieve a balanced representation among those with normal glucose levels, impaired fasting glucose, and diabetes—three pivotal indicators of cardiometabolic health.
During the follow-up period, 132 participants were diagnosed with heart failure. Statistical evaluations indicated a strong and independent link between increased waist-to-height ratios and heightened heart failure risk, even after factoring in glucose levels and other established risk contributors.
Key Findings:
– An increase of one standard deviation in waist-to-height ratio was associated with a 34% higher risk of heart failure.
– Individuals in the highest quartile for waist-to-height ratio faced a 2.7-fold elevated risk of developing heart failure compared to those in the lower three quartiles.
– The median waist-to-height ratio recorded in the study was 0.57—substantially higher than the 0.50 ratio deemed a critical risk threshold.
A Straightforward Guideline: Waist Should Be Less Than Half Your Height
In contrast to BMI, which necessitates numerical computation and can be affected by muscle mass and body structure, the waist-to-height ratio is a clear and universally applicable measure.
“Your waist should be less than half of your height,” noted Dr. John Molvin, study co-author and a physician at Malmö University Hospital. For instance, a person measuring 68 inches (5 feet 8 inches) tall should aim to have a waist circumference of less than 34 inches to remain within a healthy range.
The Significance of This Research
This new research could have significant consequences for how healthcare professionals evaluate heart failure risk and implement obesity-related interventions. It notably questions the so-called “obesity paradox,” where certain studies suggest individuals with higher BMI may achieve better outcomes post-heart failure diagnosis. Such anomalies become less perplexing when body composition and fat distribution—rather than just total body weight—are taken into account.
By prioritizing the waist-to-height ratio, healthcare providers may more effectively identify at-risk individuals, particularly those considered to have a normal BMI but who possess dangerous deposits of central fat. This could lead to more tailored treatment strategies, lifestyle changes, and monitoring practices.
Routine Waist Measurements on the Horizon?
With the waist-to-height ratio’s proven reliability, accessibility, and predictive capabilities, health researchers and clinicians are advocating for its addition to routine health examinations alongside standard measures such as blood pressure and cholesterol levels.
Dr. Jujic highlighted that consistently monitoring waist circumference in relation to height could help detect early warning signs long before heart failure symptoms manifest.
Future Directions: Expanding the Study
The Lund University researchers intend to extend their investigation to assess waist-to-height ratio as an indicator not only for heart failure but also for other significant metabolic disorders in broader and more varied populations. As obesity rates escalate globally and the prevalence of chronic cardiovascular diseases rises, identifying straightforward yet effective screening methods is increasingly essential.
A Call to Action for Public Health
Heart failure continues to be one of the primary causes of death and disability worldwide. This latest evidence urges individuals to focus more on factors beyond the scale’s reading.