Scientists have identified a unique kind of brain cell that misbehaves in mice exhibiting schizophrenia-like behavior, and when they reduced the activity of these cells, the animals’ symptoms improved. This finding indicates a specific period during brain development when medical professionals might eventually intervene to prevent cognitive issues from arising.
The relevant cells are a subgroup of inhibitory neurons known as Sst_Chodl cells. Though they represent only a minuscule part of the brain’s cellular makeup, they exert significant control over the functioning of neural circuits. In mice with a genetic deletion associated with human schizophrenia, these cells exhibited increased activity as the animals transitioned from adolescence to adulthood, leading to disruptions in their sleep patterns.
“Current treatments for cognitive symptoms in individuals diagnosed with conditions like schizophrenia are insufficient. We need to gain further insight into what leads to these cognitive symptoms which stem from developmental impairments in the brain,” states Konstantin Khodosevich, a professor at the University of Copenhagen’s Biotech Research and Innovation Center. “Our research may be a preliminary step toward a new, focused treatment that could prevent cognitive symptoms.”
A Chain That Breaks
Schizophrenia does not manifest from birth. The disorder arises from faulty brain circuitry that develops during the fetal stage, yet symptoms such as hallucinations, delusions, and cognitive impairment generally surface only in late adolescence or early adulthood. Researchers have long been baffled by this delay. Why does the brain endure developmental faults for an extended period before descending into dysfunction?
Katarina Dragicevic, one of the primary authors of the study, traced brain development from prenatal stages to adulthood in mice with a deletion in chromosome region 15q13.3. This same genetic irregularity in humans is linked to epilepsy, autism, and schizophrenia. She discovered that molecular and functional alterations were relatively minor throughout childhood. However, when the mice reached adolescence, the system began to fail.
“For an extended period, the brain can compensate for developmental mistakes and sustain relatively normal functionality. But eventually, it’s like a chain snapping: the brain can no longer adapt, and that’s when symptoms begin to appear,” Dragicevic clarifies. “However, until that moment, prevention should be achievable.”
That pre-snap timeframe may represent an ideal opportunity for intervention. If healthcare providers could identify at-risk children and stabilize their brain circuits prior to the chain breaking, they could potentially prevent years of crippling symptoms.
Sleep as a Window into Brain Disorder
Sleep issues are prevalent among individuals with psychiatric illnesses, so the team in Copenhagen utilized sleep as a behavioral indicator. They observed the mice continuously, noting when they fell asleep, the depth of their sleep, and how often they awoke. The mutant mice had poor sleep quality, waking frequently, and spending less time in restorative slow-wave sleep.
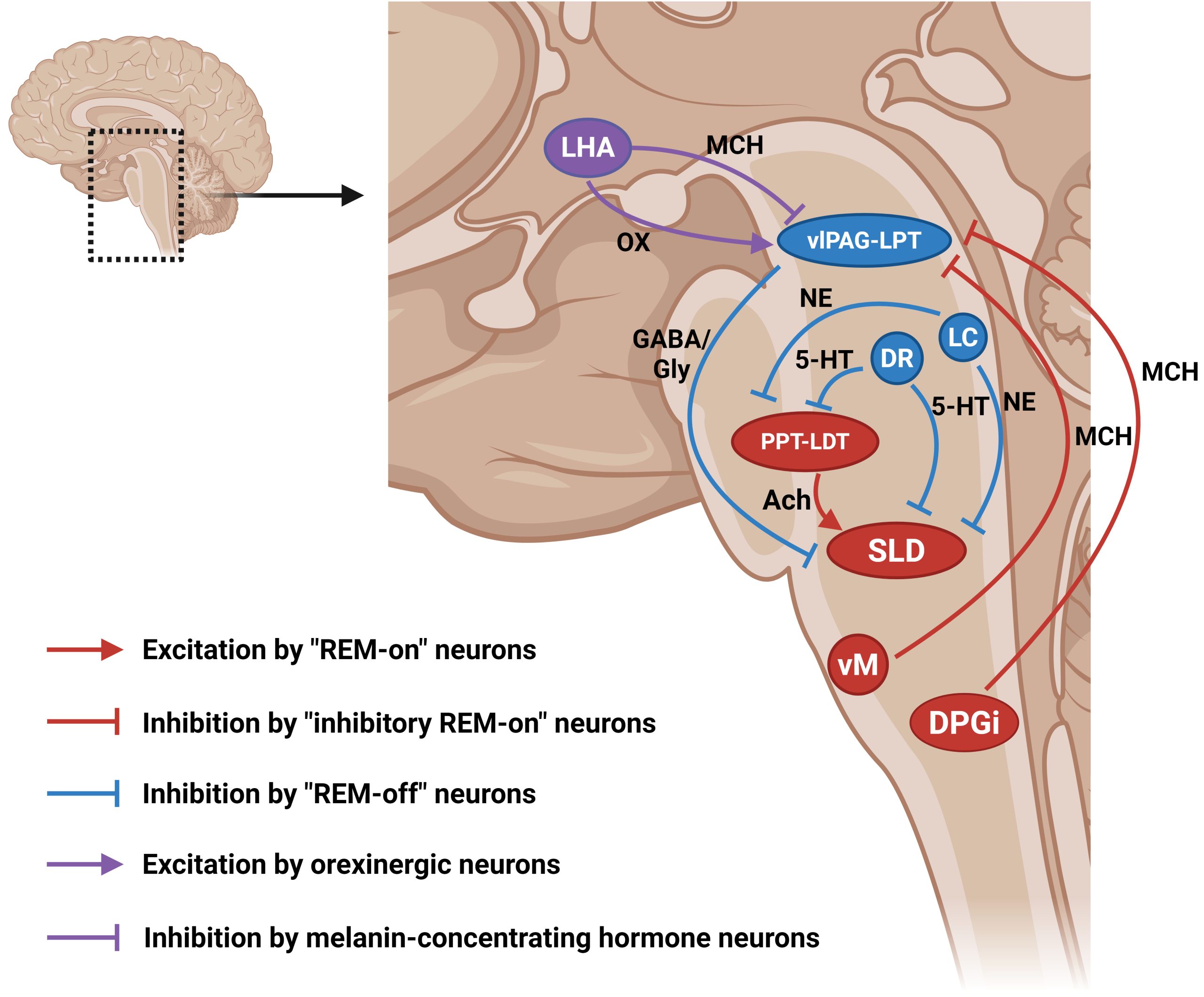
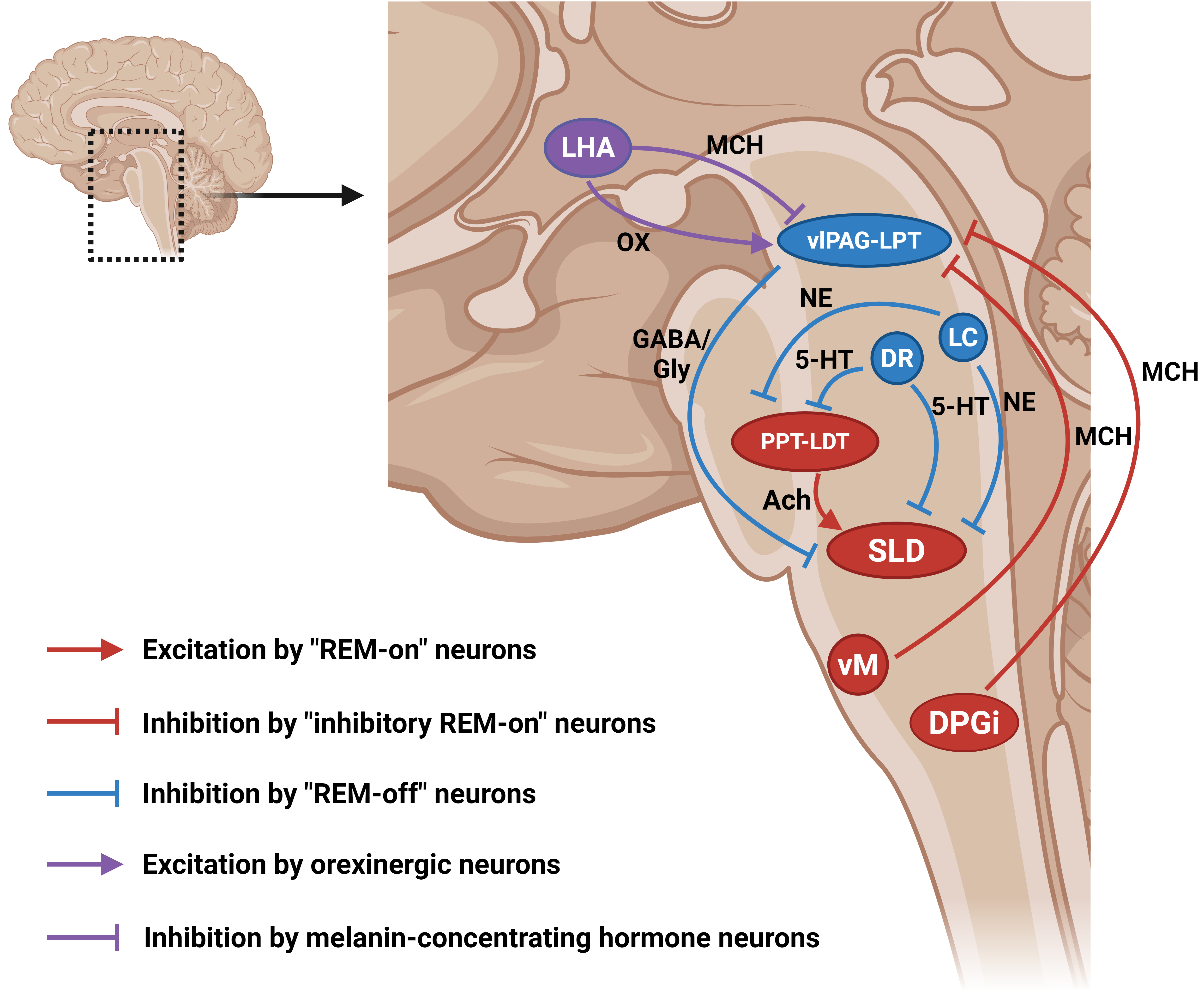
Using single-nucleus RNA sequencing, the researchers examined gene activity in thousands of individual brain cells. The method uncovered that Sst_Chodl neurons, a rare group of GABAergic cells that send signals over long distances to other brain areas, exhibited the most significant molecular disruption. These cells are intended to function as inhibitory regulators, calming overly active circuits. Instead, they were firing excessively.
Calcium imaging and patch-clamp recordings corroborated this observation. While many deep-layer somatostatin neurons displayed diminished responses, Sst_Chodl cells went against the pattern, becoming hyperactive. The researchers then utilized a method called chemogenetics to selectively silence these cells. Upon doing so, the mice’s sleep habits returned to normal.
“This indicates that this specific type of brain cell is crucial for sleep in mice with this condition,” states Navneet Vasistha, an assistant professor at the university and a primary author of the study. “Using a method called chemogenetics, we can decrease the activity of these cells and restore typical sleep patterns, potentially alleviating other psychiatric symptoms as well.”
The finding is remarkable because Sst_Chodl neurons are so uncommon. They can easily be overlooked in studies that group all inhibitory cells together, yet they seem to be vital regulators of circuit equilibrium. Their long-distance projections enable them to impact remote brain regions, making them powerful contributors to widespread dysfunction.
Translating these findings to humans will require years, if it is feasible at all. Mice are not equivalent to humans, and chemogenetics is not yet suitable for clinical application. However, the study provides a proof of concept: targeting a particular cell type can reverse a complex behavioral symptom. This stands in stark contrast to the blunt tools currently in use, which often produce side effects due to their broad impact on numerous brain regions.
“This type of cell might eventually serve as a treatment target,” Vasistha notes. “We aspire that in the future, patients will benefit from therapies for cognitive disorders that do not broadly affect brain cells, but are so specifically focused that side effects can be minimized.”
The research, published in Neuron, also emphasizes how much remains to be understood regarding the cellular foundations of psychiatric illnesses.