Surgeons undertaking hip replacements contend with a daunting statistic: almost 50% of postoperative thigh bone fractures occur within the initial three months following surgery, frequently necessitating patients’ return to the operating room. A recent 14-year analysis monitoring over 4,500 hip replacement procedures indicates that a surprisingly straightforward solution could significantly decrease this issue.
The solution, as reported by researchers at Chiba University in Japan, is found in a design element that seems almost insignificant: a compact stabilizing ring, or collar, located at the upper part of the artificial hip stem, paired with a bone-compatible coating. In direct comparisons with the smooth, wedge-shaped stems preferred by many surgeons, the collared versions demonstrated an 85% decrease in early fractures. The contrast was notable: only two fractures occurred in the collared group compared to 13 in the wedge group, even after researchers meticulously matched patients by age, weight, and health.
One Surgeon, Two Stem Designs, Clear Results
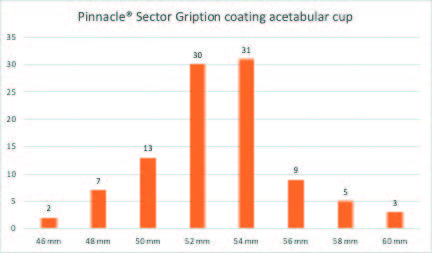
What renders this study particularly persuasive is its methodology. Instead of comparing outcomes across various hospitals or surgeons, which could cloud the results due to differing techniques and patient selections, lead researcher Rui Hirasawa and his team examined 4,511 procedures administered by a single surgeon at one medical facility from 2009 to 2023. They utilized propensity score matching, a statistical approach adapted from economics, to form two groups of 1,804 patients each, who were virtually indistinguishable in all measurable aspects except for the type of implant received.
The collared stems are equipped with a ring that directly contacts the patient’s bone, offering immediate mechanical support. Furthermore, they are entirely coated with hydroxyapatite, a calcium-based substance that promotes the patient’s bone to grow directly onto the implant surface. In contrast, the flat-tapered wedge stems depend solely on their shape and snug fit within the bone canal for stability. No collar, no coating, just geometry and friction.
“Drawing from both our clinical experiences and literature suggesting a decreased prevalence of post-THR femoral fractures with collared fully HA-coated stems, we were motivated to explore whether these stems could indeed lessen the chance of such fractures.”
The researchers disclosed their findings in the October 2025 edition of the Bone & Joint Journal, with implications that reach far beyond Japan. With approximately one million total hip replacements conducted globally each year, even modest percentage enhancements in safety can translate to thousands of patients who might evade a severe complication.
The Tradeoff Surgeons Need to Know
However, before orthopedic surgeons hasten to change implant types, a caveat exists. The study revealed that collared stems were linked to a higher incidence of fractures during surgery itself, specifically as the surgeon is inserting the implant into the bone. These intraoperative fractures can typically be addressed immediately with wires or screws, but they complicate the procedure and necessitate meticulous technique.
This observation indicates that the collared design requires greater precision during insertion, possibly due to the collar making it more challenging to adjust the implant’s position once it begins to be inserted. Hirasawa and his colleagues stress that further research is essential to refine surgical techniques specifically for collared stems and to determine which patients are most suited to each design.
The stakes are significant. Femoral fractures following hip replacement are currently the primary cause of revision surgery, a process that is physically taxing for patients and immensely expensive for healthcare systems. Many of these patients are elderly, often with other health complications that increase the risks of any additional surgery. Preventing even a single fracture could mean the distinction between a patient reclaiming their independence or facing lasting disability.
“Our findings hold the potential to directly enhance patient safety and surgical outcomes in THR by assisting surgeons in making more informed implant choices, resulting in fewer serious complications, quicker functional recovery, and a reduced necessity for reoperation.”
Hirasawa envisions that this research could eventually establish a new global benchmark for implant selection. For now, it provides surgeons with tangible data to consider the tradeoffs: a design that is slightly more complex to insert but considerably less likely to result in failure during the critical early months when patients are attempting to rebuild their lives, one cautious step at a time.
The Bone & Joint Journal: [10.1302/0301-620X.107B10.BJJ-2024-1494.R1](https://doi.org/10.1302/0301-620X.107B10.BJJ-2024-1494.R1)
There’s no paywall here
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!