A subtle signal in the bloodstream could indicate a story unfolding decades in the future. In a comprehensive 25-year analysis involving approximately 6,000 British civil servants, researchers from UCL found that elevated midlife levels of cardiac troponin I, a marker indicative of minimal heart damage, were associated with accelerated cognitive decline, reduced brain volumes in MRI scans, and an increased likelihood of dementia as one ages.
This study, published in the European Heart Journal, monitored participants who were free from cardiovascular issues and dementia at the start, aged between 45 and 69. Utilizing a high-sensitivity assay, the research team measured troponin across three different time intervals and evaluated cognitive abilities through six rounds of testing. Every doubling of troponin correlated with a 10% rise in dementia risk, and individuals who began within the highest troponin bracket had a 38% elevated risk compared to those beneath the assay’s quantification limit. In a brain imaging sub-study, higher initial troponin levels were linked to diminished grey matter volume and extensive hippocampal atrophy approximately 15 years later.
The signal appeared to arise well in advance of any symptoms. In a nested case-control study, individuals who eventually developed dementia exhibited consistently higher troponin levels compared to matched counterparts from 7 to 25 years before their diagnosis. The trend, according to the authors, implies that subclinical myocardial injury could play a role in a causal pathway, affecting cerebral perfusion and vascular health over an extended preclinical period.
Cardiac troponin I is primarily recognized as a diagnostic indicator during suspected heart attacks, where levels surge. However, in the lower, asymptomatic range now detected through high-sensitivity assays, troponin may indicate ongoing micro-injuries or cardiac dysfunction. Envision an unseen signal from the heart, with a few molecules emitted at a time, signaling stress on tissues that might also foreshadow strain on the brain’s intricate networks.
“Compromised heart health during middle age increases the risk of dementia later in life.”
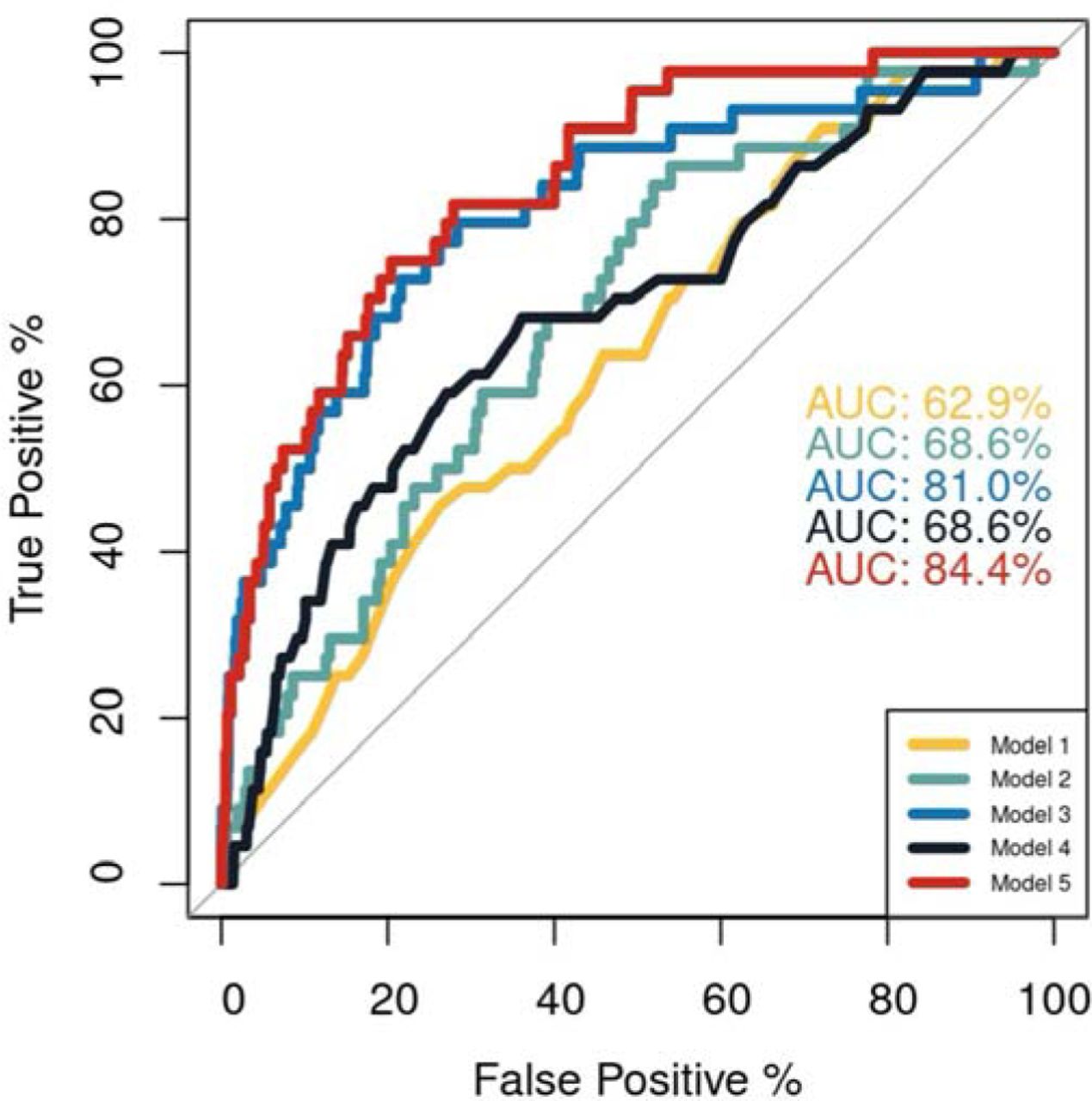
The epidemiological foundation of the study is robust. Participants were drawn from the established Whitehall II cohort, with dementia outcomes verified through linked UK health records up until March 2023. Even after adjusting for demographic elements and primary cardiovascular risk factors, the associations remained significant. Cognitive paths diverged with age: at ages 60 and 70, group scores appeared similar, but by ages 80 and 90, those with higher midlife troponin levels showed significantly poorer performance, roughly equating to being 1.4 to 2 years older in cognitive terms.
Insights from Brain Imaging
Among 641 participants who underwent MRI scans, higher initial troponin corresponded with reduced grey matter volume and increased hippocampal atrophy after approximately 15 years. The magnitude of the effect aligned with aging: the reduction in grey matter within the highest troponin group mirrored nearly 2.7 years of additional aging, with hippocampal atrophy resembling about 3 years. White matter hyperintensities did not show a significant correlation, although diffusion metrics suggested potential microstructural alterations. The imaging results support a vascular-neurodegenerative overlap hypothesis, where subpar cardiac function reduces cerebral blood flow and accelerates tissue loss in regions with high metabolic requirements.
Critically, the troponin indicator was not exclusive to those with overt heart disease. Researchers eliminated participants with baseline cardiovascular disease and accounted for blood pressure, cholesterol levels, diabetes, obesity, smoking, and physical activity. Sensitivity analyses considering APOE genotype and kidney function yielded consistent results. While this resilience does not confirm causation, it raises the possibility of troponin serving as a midlife biomarker for assessing brain risk, alongside conventional metrics.
“Brain damage evident in those with dementia accumulates gradually over decades before symptoms emerge.”
Transitioning from Risk Assessment to Action
Could troponin assist in developing a practical dementia risk assessment in clinical settings? The authors believe so, yet underscore the need for further validation. High-sensitivity assays are widely available, and moderately elevated levels in otherwise healthy individuals might indicate who could gain the most from proactive risk management. The Lancet Commission’s 2024 estimate suggests that 17% of dementia cases could be preventable by addressing cardiovascular risks such as hypertension, lipid levels, physical inactivity, and obesity. Troponin could help pinpoint that prevention window when it’s most crucial, in one’s 40s, 50s, and 60s, before cognitive trajectories start to diverge.
The study does have limitations. It is observational, primarily involving White participants, and focused on civil servants, which could restrict its applicability. Changes in dementia policies and diagnostic criteria over the past two decades may affect the timing of recorded diagnoses. Additionally, while troponin indicates risk, it does not elucidate mechanisms. Nonetheless,