Most individuals possess a genetic variant that experts have traditionally regarded as benign. According to a comprehensive new study, this belief may have been a significant error.
Researchers from University College London and the University of Eastern Finland now suggest that between 72% and 93% of Alzheimer’s disease cases would not materialize without the impact of two prevalent variants of the APOE gene. This discovery shifts the perspective on a molecule that has been under examination for thirty years from a significant risk factor to something akin to a master regulator of the disease.
The research team arrived at this conclusion after evaluating genetic and clinical information from over 450,000 individuals across four major international studies, including UK Biobank, FinnGen, a substantial U.S. amyloid imaging trial, and a dataset where Alzheimer’s was confirmed through brain tissue analysis post-mortem. In that last cohort, where diagnostic certainty was greatest, the prevalence of the disease linked to APOE reached 92.7%.
The Subtle Influencer
APOE exists in three primary variants. The ε4 variant has been acknowledged as harmful since the 1990s, significantly heightening Alzheimer’s risk for those who possess it. The rare ε2 variant provides protective benefits. However, ε3, which is carried by roughly 95% of the global population, has usually been perceived as neutral.
This perceived neutrality seems to be misleading. By utilizing individuals with two copies of ε2 as a low-risk reference point—something only feasible with such extensive datasets—the researchers revealed that ε3 considerably elevates Alzheimer’s risk compared to ε2. This variant is not merely an observer; it acts as a subdued contributor whose widespread impact eclipses that of its more infamous counterpart because so many individuals carry it.
The investigation also discovered that around 45% of cases of all-cause dementia are associated with these identical genetic variants. No other known genetic marker for Alzheimer’s or even heart disease carries such an extensive attributable fraction of total disease burden.
Interestingly, the protein produced by APOE aids in cholesterol transportation within the brain. The rationale behind evolution maintaining variants that increase dementia risk remains uncertain.
Implications for Treatment
The researchers emphasize that genetics does not equate to fate. Even among individuals with two copies of ε4, the highest-risk scenario, the lifetime risk of Alzheimer’s remains under 70%. Factors such as smoking, elevated cholesterol, social isolation, and other influences still play a role in whether the disease manifests. The gene induces vulnerability, but other elements take advantage of it.
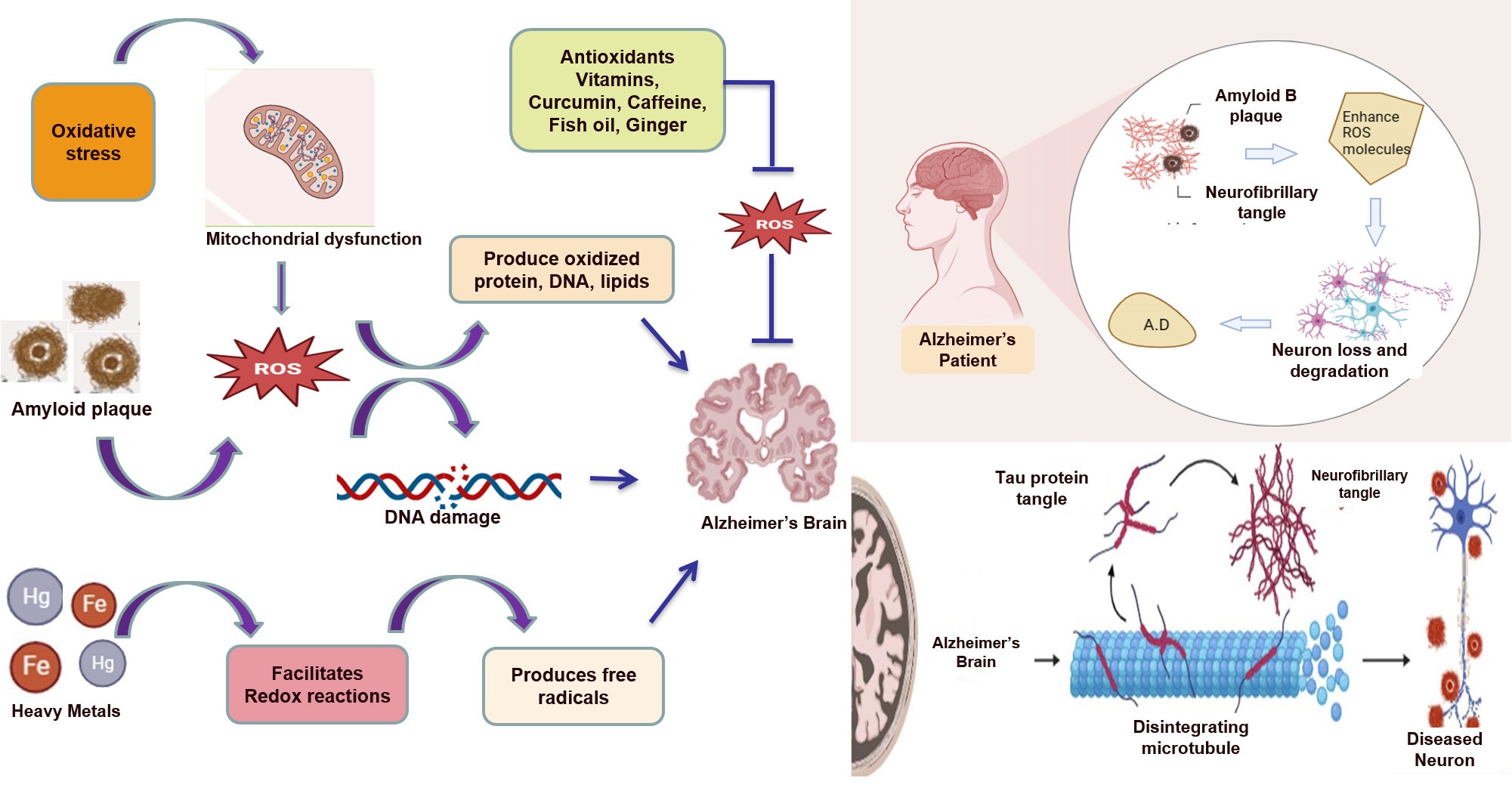
Nevertheless, the primary implication is hard to overlook. In spite of decades concentrating on amyloid plaques and tau tangles, very few therapies currently in clinical trials directly address APOE or its downstream biology. The authors of the study contend this indicates a lost opportunity.
“We have long underrated how significantly the APOE gene contributes to the Alzheimer’s disease burden,” comments Dylan Williams from University College London. “Much of the disease would not exist without the added influence of the common ε3 allele.”
Recent progress in gene therapy and drugs targeting proteins make APOE a viable focus. Researchers are already investigating treatments that replicate the protective effects of ε2 or neutralize the hazards presented by ε3 and ε4. Should these interventions prove successful, data indicates they could potentially eradicate the majority of Alzheimer’s cases before they ever arise.
The findings were remarkably consistent across all four datasets, despite variations in how Alzheimer’s and dementia were defined. The researchers point out that this consistency bolsters confidence that the role of APOE is not an artifact of any single study’s methodology. The gene’s influence seems essential to the disease itself.
[npj Dementia: 10.1038/s44400-025-00045-9](https://doi.org/10.1038/s44400-025-00045-9)
There’s no paywall here
If our reporting has informed or inspired you, please consider contributing. Every donation, no matter how small, helps us continue to deliver accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for supporting us!