Approximately 40 percent of individuals with advanced melanoma observe their tumors evolve and spread despite immunotherapy, frequently to the lungs, where cancer cells develop molecular defenses that keep the body’s immune system at bay. The issue isn’t that checkpoint inhibitors are entirely ineffective. It’s that tumors learn to inhibit immune responses through various pathways simultaneously, and targeting just one seldom resolves the issue.
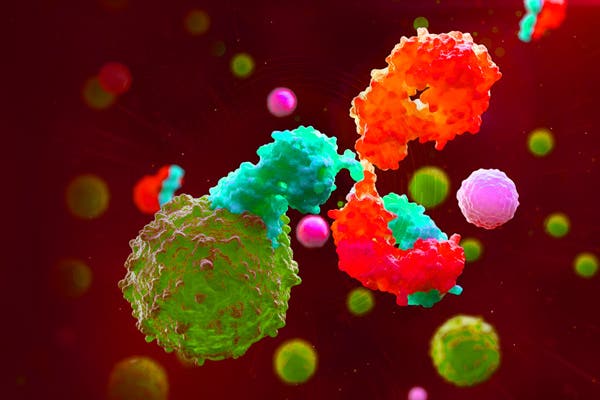
Engineers from Columbia University have reported an inhalable treatment aimed at directly overcoming that resistance within lung tissue. This system employs exosomes, nanoscale vesicles naturally produced by the body, to deliver two therapeutic proteins concurrently. One inhibits the PD-1 or PD-L1 checkpoint pathway responsible for silencing T cells. The other disrupts Wnt or beta-catenin signaling, which physically blocks immune cells from infiltrating tumors. This research, led by biomedical engineer Ke Cheng, has been published in Nature Biotechnology.
Conventional antibody drugs travel through the bloodstream and may fail to reach tumors in the right amounts or at the same time. By co-displaying both proteins on a single exosome using a sorting domain known as Alix, the researchers ensured that each carrier transmits a synchronized signal in a precise one-to-one ratio. When inhaled, the modified exosomes adhere to lung tissue significantly better than intravenous antibodies, concentrating precisely where metastases are likely to occur.
Mobilizing Killers, Minimizing Unintended Harm
In mouse models of metastatic melanoma that had ceased responding to checkpoint inhibitors, the inhaled treatment fully reversed resistance. The intervention attracted cancer-killing CD8 T cells into tumors and diminished indications of immune fatigue. Notably, local delivery meant that the therapy did not circulate throughout the body, which can trigger autoimmune toxicity, a frequent concern with systemic immunotherapies that broadly stimulate immune responses.
The team assessed the method across four types of resistant melanoma, including a humanized model utilizing patient-derived tumors. In every instance, the bispecific exosomes surpassed dual-antibody therapies. The treatment also inhibited tumors in the liver, indicating that the platform might be effective beyond lung metastases. Safety evaluations revealed no observable liver or kidney damage in mice.
“The tandem exosome engineering technique provides a novel way to deliver multiple therapeutic proteins locally, a platform that could apply to autoimmune, infectious, or fibrotic conditions where multi-target modulation is essential,” Ke Cheng states.
Future Directions
This research remains in the preclinical stage. Cheng’s team highlights that larger animal studies, formal toxicology evaluations, and preparations for early-phase human trials lie ahead. The approach reconceptualizes drug resistance not as a single barrier to breach but as a system that may need to be disabled simultaneously.
Immune checkpoint inhibitors operate by releasing molecular brakes that usually prevent immune cells from attacking healthy tissue. Cancer cells exploit these same brakes to evade detection. When tumors develop resistance, they frequently activate additional suppression pathways, resulting in a layered defense. The BEAT system, short for bispecific exosome activator of T cells, addresses this issue by simultaneously releasing the brakes on immune cells and unlocking the doors that keep them from infiltrating tumors.
If this strategy is successful in humans, inhalable multi-target therapies could revolutionize how clinicians tackle cancers that have learned to conceal themselves effectively. For patients whose melanoma no longer responds to current top treatments, this localized nanotherapy offers a new tactical choice, one that focuses efforts directly where the disease entrenches itself.
Nature Biotechnology: 10.1038/s41587-025-02890-8
There’s no paywall here
If our reporting has provided you with valuable insights or inspiration, please consider making a donation. Every contribution, regardless of size, empowers us to continue delivering accurate, engaging, and reliable science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep revealing the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!