**Utilizing Monoclonal Antibodies Against Epstein-Barr Virus: A New Era in Transplant Medicine**
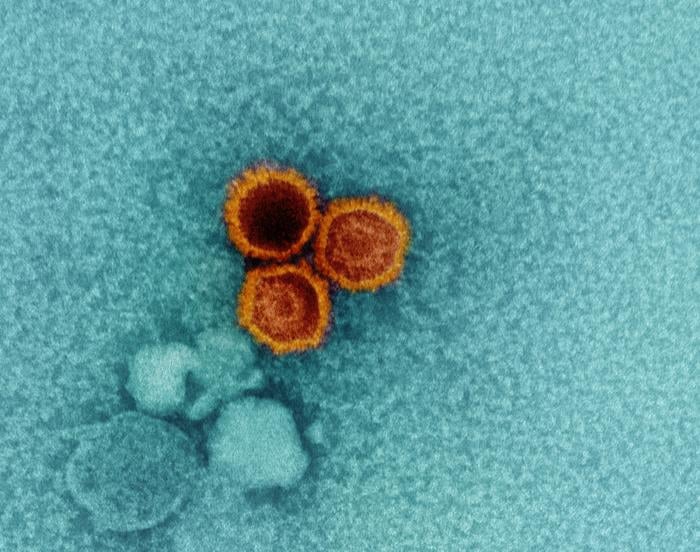
The Epstein-Barr virus (EBV) is an omnipresent pathogen, with an alarming 95% of the worldwide population harboring it asymptomatically. Most individuals remain unaware of its existence, living symptomless lives. However, for those with weakened immune systems, particularly transplant recipients, EBV represents a serious danger. In these patients, the virus can reactivate, potentially resulting in fatal outcomes, such as post-transplant lymphoproliferative disorder.
Developing a treatment for EBV has perplexed researchers for many years. Traditionally, the virus’s intricate mechanism of attaching to nearly all B cells has complicated efforts to create effective antibodies. This interaction conceals glycoproteins gp350 and gp42, which are essential for the virus’s entry and fusion with host cells. Overcoming this adaptive disguise was like attempting to find a specific person in a crowd of identical faces.
The group at Fred Hutchinson Cancer Center has made a significant advancement. By utilizing transgenic mice from Alloy Therapeutics, designed to produce humanized antibodies, researchers navigated past obstacles. These mice, equipped with human antibody genes, were vaccinated against EBV’s critical proteins, gp350 and gp42. This undertaking resulted in ten powerful antibody candidates.
Among these, the antibody ATX-42-2 rose as a leading candidate, precisely targeting gp42’s fusion abilities. When evaluated in humanized mice, ATX-42-2 showed outstanding effectiveness in blocking EBV infection—none of the treated mice showed viral DNA in their spleens, starkly contrasting with the control group, which exhibited significant infection indicators.
Vital structural details further clarify how ATX-42-2 functions, disrupting the viral entry mechanism by obstructing gp42 interactions on B cells. This not only provides a viable avenue for treatment but also establishes a foundation for potential EBV vaccines.
The implications are significant, especially for the approximately 128,000 transplant patients in the US each year. Effective management of EBV is a noteworthy unmet requirement in transplant medicine. Approaches like pre-transplant antibody infusions could act as a preventive measure, lowering the risk of EBV-related complications.
Although these results signify a major step forward, challenges persist. The mouse model studies highlighted the necessity for continued strategies targeting sustained coverage and defense against EBV’s comprehensive range of cell targets beyond B cells. Existing data indicate that antibody combinations or modifications to prolong antibody half-life could improve therapy longevity and efficiency.
In conclusion, this research signals a hopeful chapter in EBV treatment development. Genetically engineered human monoclonal antibodies that effectively neutralize EBV, validated in animal studies and ready for clinical trials, represent a milestone in this protracted scientific journey. As Dr. McGuire from Fred Hutch expresses, the momentum created by these results could soon evolve into groundbreaking clinical applications, providing hope to the most at-risk patients maneuvering through the delicate realm of transplant medicine.